The role of platelets in the pathogenesis of acute coronary syndrome (ACS) is well recognized.1 Persistent platelet activation despite antithrombotic therapy has an influence on the severity of ischemic cardiomyopathy.
Reticulated platelets are the youngest form of circulating platelets. They are larger than senescent platelets, contain residual RNA that confers a reticulated appearance, and are hemostatically more active because they express more glycoprotein Ib and IIb/IIIa receptors. Currently, a fast, automated method is available to quantify reticulated platelets by the immature platelet fraction (IPF), calculated as the ratio between immature platelets and total platelets.
The mean platelet volume is an indicator of platelet reactivity. An elevated mean platelet volume in the acute phase of myocardial infarction is associated with a poorer short-term prognosis.2 IPF determination may be more sensitive and specific than the mean platelet volume for evaluating platelet reactivity.3 It has been observed that, in patients with coronary disease, the IPF is elevated relative to the healthy population,4 and it is also increased in ACS with respect to stable coronary disease.5
In our study, reticulated platelets were analyzed by plasma IPF determination in hospitalized ACS patients with the aim of determining the short-term prognostic value (predictor of in-hospital mortality) of this parameter.
Between January 2007 and April 2008, 251 hospitalized ACS patients were studied. ACS was established based on symptoms of myocardial ischemia in the 24h prior to admission together with elevated cardiac biomarkers and/or electrocardiographic abnormalities (ST deviation≥0.5 mm and/or T wave changes, consisting of negative T waves≥2 mm in 2 or more contiguous leads). The sample for IPF determination was obtained in the morning of the first day of hospitalization. IPF was determined with a Sysmex XE-2100 automated hematology analyzer (Sysmex; Kobe, Japan), which, in relation to the platelet volume and RNA content, distinguishes the percentage of immature platelets.
A descriptive statistical analysis was performed. We calculated descriptive statistics of frequency of the continuous variables studied (median [interquartile range]) and the categorical variables (percentages). The Mann-Whitney U test was used to compare quantitative variables, and the Pearson chi-square test to determine associations between qualitative variables. The predictive factors of in-hospital mortality were established by univariate analysis, and statistically significant variables were included in a binary multivariate logistic regression analysis. All statistical analyses were carried out with the IBM SPSS Statistics 18 program. Statistical significance was set at a P-value of<.05.
The characteristics of the study population are shown in Table 1. The comparison of IPF values in ACS patients with and without ST segment elevation showed no significant differences between the 2 groups: 5.20% [3.60%-7.60%] vs 4.75% [3.12%-7.42%] (P=.289). Thirty-one patients (12.3%) died during hospitalization. The IPF value was higher in patients who died than in those who survived: 6.60% [4.20%-10.80%] vs 4.80% [3.10%-6.95%] (P=.002). In-hospital mortality increased as the IPF tertile increased, such that the probability of death was higher in patients in the third tertile (IPF>6.2%) than in those in the first (IPF<3%) (22% vs 6%; P=.003). Mortality observed in the high-risk group determined by the global registry of acute coronary events (GRACE) risk score (≥140) was 10%, 15.7%, and 25% (P=.148) for the first, second, and third IPF tertiles, respectively, and in the non-high-risk group (GRACE score<140), mortality was 2.3%, 3.1%, and 15.3% (P=.057) for the first, second, and third tertiles, respectively.
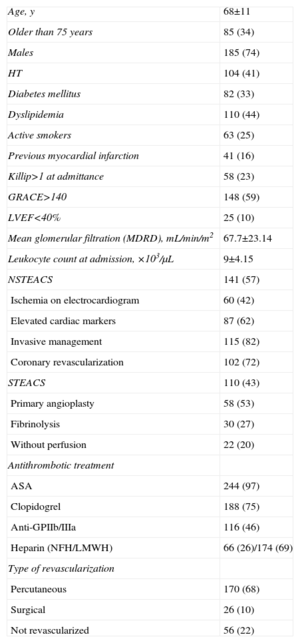
Characteristics of the Population.
| Age, y | 68±11 |
| Older than 75 years | 85 (34) |
| Males | 185 (74) |
| HT | 104 (41) |
| Diabetes mellitus | 82 (33) |
| Dyslipidemia | 110 (44) |
| Active smokers | 63 (25) |
| Previous myocardial infarction | 41 (16) |
| Killip>1 at admittance | 58 (23) |
| GRACE>140 | 148 (59) |
| LVEF<40% | 25 (10) |
| Mean glomerular filtration (MDRD), mL/min/m2 | 67.7±23.14 |
| Leukocyte count at admission, ×103/μL | 9±4.15 |
| NSTEACS | 141 (57) |
| Ischemia on electrocardiogram | 60 (42) |
| Elevated cardiac markers | 87 (62) |
| Invasive management | 115 (82) |
| Coronary revascularization | 102 (72) |
| STEACS | 110 (43) |
| Primary angioplasty | 58 (53) |
| Fibrinolysis | 30 (27) |
| Without perfusion | 22 (20) |
| Antithrombotic treatment | |
| ASA | 244 (97) |
| Clopidogrel | 188 (75) |
| Anti-GPIIb/IIIa | 116 (46) |
| Heparin (NFH/LMWH) | 66 (26)/174 (69) |
| Type of revascularization | |
| Percutaneous | 170 (68) |
| Surgical | 26 (10) |
| Not revascularized | 56 (22) |
ASA, acetylsalicylic acid; GPIIb/IIIa, glycoprotein IIb/IIIa; LMWH, low molecular weight heparin; HT, hypertension; LVEF, left ventricular ejection fraction; MDRD, modified diet in renal disease; NFH, non-fractionated heparin; NSTEACS, non-ST-segment elevation acute coronary syndrome; STEACS, ST-segment elevation acute coronary syndrome.
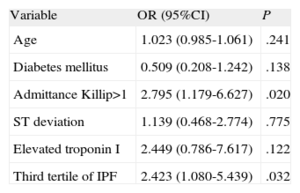
After adjusting for other covariables (age, diabetes mellitus, heart failure at hospitalization, ST deviation on electrocardiographic study, and troponin elevation) multivariate analysis showed that the third tertile of IPF remained as an independent predictor of in-hospital mortality: odds ratio=2.42 (95% confidence interval, 1.08-5.43; P=.032) (Table 2).
Multivariate Analysis of In-hospital Mortality.
| Variable | OR (95%CI) | P |
| Age | 1.023 (0.985-1.061) | .241 |
| Diabetes mellitus | 0.509 (0.208-1.242) | .138 |
| Admittance Killip>1 | 2.795 (1.179-6.627) | .020 |
| ST deviation | 1.139 (0.468-2.774) | .775 |
| Elevated troponin I | 2.449 (0.786-7.617) | .122 |
| Third tertile of IPF | 2.423 (1.080-5.439) | .032 |
95%CI, 95% confidence interval; IPF, immature platelet fraction; OR, odds ratio.
Our study has 2 main limitations. The first is possible selection bias, since the IPF was determined in the first morning blood test following hospitalization, and this sample is collected in patients at highest risk. Hence, our results would be valid for this population. The second limitation is the small sample size and limited number of adverse events, which impedes precise adjustment for all the variables potentially related to mortality, and limits the robustness of the results.
Therefore, we conclude that in patients hospitalized for ACS, elevated IPF values determined in the first 24 h following admission are associated with a poorer in-hospital prognosis due to an increase in mortality, even among patients who are not considered at high-risk according to the GRACE score. These patients, who can be identified by standard blood testing, may benefit from more intensive medical treatment or use of a prompt revascularization strategy. Future studies should confirm the association between IPF and mortality and investigate the pathophysiology of these findings.
.