A 65-year-old woman, resident of Mexico City, began to complain of myalgia, headache, general malaise, and fever 3 days after returning from a 5-day stay in Acapulco. Two days later, she experienced syncope and was taken to hospital. She was conscious, her blood pressure was 70/30mmHg, respiratory rate was 24 per minute, and her temperature was 38.6°C; no skin lesions or edema where seen, heart sounds were normal, and lung fields clear.
Her electrocardiogram showed sinus rhythm; chest x-ray was normal. A complete blood count revealed normal hemoglobin, normal white blood cells with 90% neutrophils, and mild thrombocytopenia. Blood urea nitrogen and creatinine were normal; hyponatremia and hypokalemia were also present (126 and 3.6 mEq/L, respectively).
Volume replacement was started with saline and norepinephrine infusion was also required. Clarithromycin, cefepime, and oseltamivir were started. The patient continued to have a fever of 38.7°C and increased hemoglobin and hematocrit (17.9g/dL and 53%) and leucopenia (3000/mL3 with 71% neutrophils, 17% lymphocytes, and 12% monocytes) were observed. All culture samples were negative.
On the sixth hospital day, she suddenly developed oppressive chest pain and dyspnea. Heart sounds revealed S3 gallop rhythm and generalized lung rales. An electrocardiogram showed sinus tachycardia, new ST depression in V1 through V3, and ST elevation in aVR and aVL. Chest x-ray revealed an enlarged cardiac silhouette and pulmonary edema. Creatine kinase-MB fraction was elevated (38mg/dL), while troponin I was normal (1.6μg/L).
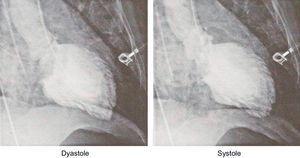
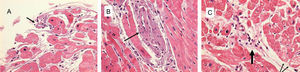
The patient was started on noninvasive ventilation, digoxin, furosemide and ivabradine. Six hours later she developed bidirectional ventricular tachycardia, sustained monomorphic ventricular tachycardia, and polymorphic ventricular tachycardia, which were attributed to digitalis intoxication and were resolved with diphenylhydantoin. Endotracheal intubation was required and cardiac catheterization was performed. Left ventricular end-diastolic pressure was 38mmHg, left ventriculography demonstrated severe diffuse hypokinesis with an ejection fraction of 14% and grade II mitral regurgitation (Figure 1). Coronary angiography revealed normal coronary arteries; left ventricular endomyocardial biopsy shows necrosis of myocardial fibers (Figure 2).
Left ventricle endomyocardial biopsy (Masson 40x) shows necrosis of myocardial fibers (arrow in A) with inflammatory cell infiltration and marked interstitial edema causing fiber separation (A), perivascular inflammatory infiltrate (arrow) with a necrotic fiber (B), and perivascular lymphocytic infiltrate (thick arrow in C), and vacuolization of myocardial fibers corresponding to cellular edema (narrow arrows in C).
Dengue virus-specific IgM and IgG antibodies were positive. Oseltamivir was replaced with ribavirin. A diagnosis of severe dengue myocarditis was made and steroid treatment was initiated with methylprednisolone (500mg i.v. bolus followed by 250mg tid for 3 days).
On the tenth day, her electrocardiogram showed sinus rhythm, giant T wave inversion, and prolonged QT interval; chest x-ray showed reduction of cardiac silhouette and a marked decrease of pulmonary interstitial edema. Catecholamine infusion was stopped on the eleventh day. On the following day, the echocardiogram demonstrated normal heart dimensions and ejection fraction of 67%. On day thirteen, she was discharged.
The occurrence of hemodynamic collapse in dengue represents one of the most severe manifestations of dengue shock syndrome,1 which occurs as a consequence of an abruptly increased vascular permeability mediated by activation of cytokines, tumor necrosis factor-alpha, interleukins-6, -13 and -18, and cytotoxic factors that lead to profuse interstitial plasmatic leakage.2
Our patient had syncope, probably due to severe hypotension as documented on admission. This was initially corrected with volume3 and amine infusion. Nonetheless, hemoconcentration resulted and although there was mild thrombocytopenia she did not develop hemorrhagic complications. Following the initial hypovolemic shock, marked hypotension recurred as a consequence of severe myocarditis, which resolved following antiviral therapy and high-dose parenteral methylprednisolone, as previously reported.3
It has been suggested that dengue myocarditis can be the result of a direct viral invasion or of the immunologic response mediated by cytokines through complement activation.3 At the onset of this patient's present illness, there was no apparent myocardial involvement. It was only 6 days later, when she complained of chest pain associated with pulmonary edema, new electrocardiogram changes, and mild enzyme elevation that there was clear evidence of myocardial compromise. Coronary arteries were normal on angiography, left ventriculography demonstrated severely reduced ejection fraction and changes that have been described as a sign of myocardial necrosis; this so-called “myocardial waffling” corresponds to the furrowed appearance that was clearly identified in the ventricular edges, sparing only the basal segments. The mechanism for this phenomenon has not been clarified but could be secondary to gross myofibrillar derangement and possibly edema.4
The histological findings in this patient demonstrated myocardial fiber necrosis, marked interstitial edema and significant lymphocytic infiltration. The myocardial injury sustained by this patient proceeded with abrupt onset and extreme severity. Interestingly, fulminant cases of nondengue myocarditis such as this have a more favorable long-term outcome than those with a nonfulminant presentation.5
In addition, this patient does not adhere to the predictive variables for high mortality, as identified by Kinderman et al.6 These authors found that poor functional class, positive histological findings, and the absence of beta-receptor antagonist therapy are predictors of high mortality.