The reduction of low-density lipoprotein (LDL) concentrations through treatment with statins decreases the risk of cardiovascular events. However, in the studies carried out to examine this question, this decrease was never greater than 37%.1 The remaining or residual risk encompasses not only the traditional risk factors but also the additional modification of lipids. In this respect, the study of low high-density lipoprotein (HDL) levels as a predictor of cardiovascular events is an emerging area of interest,2 even in patients with low LDL concentrations, as they play a fundamental role in acute coronary syndrome.3 In contrast, there are very few predictors of reinfarction over the long term, especially with regard to biochemical variables, and those identified to date are epidemiological or are related to risk factors.4 The objective of this report was to evaluate the association between HDL concentrations obtained during the hospital stay in patients admitted for ST-segment elevation acute coronary syndrome and reinfarction over the long term.
For this purpose, we performed a prospective study that consecutively included all the patients discharged from a tertiary hospital after ST-segment elevation acute coronary syndrome between November 2000 and May 2004. Standard epidemiological, laboratory, and treatment variables were recorded, including those related to prognosis and plasma lipoproteins, determined within the first 24-72h after hospital admission.
Categorical variables were evaluated using the chi-square and Fisher tests; continuous variables were compared with Student's t test and analysis of variance. The population was divided into tertiles according to the HDL concentration. The association between HDL levels (tertiles T1, T2, and T3) and reinfarction was evaluated using Cox regression analysis adapted for competing events (considering this event to be death); in the initial analysis, we included those variables found to be significant in the univariate model and those that could have a plausible etiological implication for the dependent variable, independently of the P-value. The analysis was carried out using STATA 11.0. A P-value <.05 was considered to indicate statistical significance.
The study population consisted of 507 patients with a mean age of 64.4 (12.9) years, 75.7% of whom were men; 39.2% had a history of dyslipidemia, 34.9% of diabetes mellitus, 55.2% of hypertension, and 21.7% of ischemic heart disease.
The sample was divided into tertiles according to the HDL level (T1, <33mg/dL; T2, 33-40mg/dL, and T3, >40mg/dL), and it was observed that most of the patients in the lowest tertile (T1) were men, and that, overall, they were younger, had lower LDL levels, were less likely to have a history of dyslipidemia, and were more likely to be active smokers (Table).
Baseline Characteristics of the Patients According to the Serum High-density Lipoprotein Concentration Divided Into Tertiles
| T1 (HDL<33 mg/dL) | T2 (HDL 33–40 mg/dL) | T3 (HDL>40 mg/dL) | P | |
| Baseline characteristics and cardiovascular risk factors | ||||
| Age, years | 62.1 (13) | 64.7 (12.3) | 66.4 (13.1) | .007 |
| Men | 86.4 | 78.1 | 62.7 | <.001 |
| Smokers | 54.4 | 43.8 | 37.3 | .002 |
| Ex-smokers | 20.1 | 23.7 | 16 | ns |
| Hypertension | 59.2 | 53.8 | 52.7 | ns |
| Dyslipidemia | 31.4 | 44.4 | 42 | .031 |
| Diabetes mellitus | 36.1 | 34.9 | 33.7 | ns |
| PHIHD | 20.1 | 19.5 | 25.4 | ns |
| Laboratory values on admission | ||||
| Cholesterol, mg/dL | 169.6 (37.2) | 186.4 (39.2) | 199.6 (38.8) | <.0001 |
| LDL, mg/dL | 112.5 (30.9) | 123.3 (34.6) | 126.5 (33.1) | <.0001 |
| HDL, mg/dL | 28.2 (3.7) | 36.2 (2.1) | 47.4 (7.8) | <.0001 |
| Triglycerides, mg/dL | 153.3 (87.3) | 136.6 (57.9) | 128.3 (48.6) | .003 |
| Glucose, mg/dL | 132.8 (55.3) | 129.2 (53.9) | 127.8 (52.9) | ns |
| Features of the acute coronary syndrome | ||||
| Killip class on admission | 1.43 (0.77) | 1.28 (0.61) | 1.33 (0.69) | ns |
| Troponin, ng/L | 66.3 (38.7) | 55.2 (44.1) | 51.9 (39.8) | .003 |
| Lymphocytes, % | 18.5 (13.9) | 20.9 (8.5) | 18.5 (8.6) | .065 |
| Treatment at discharge | ||||
| Statin at discharge | 42.3 | 56.8 | 55.4 | .013 |
| Antiplatelet agent at discharge | 95.9 | 95.3 | 98.8 | ns |
| Beta blocker | 49.7 | 52.7 | 49.1 | ns |
| Long-term outcome | ||||
| Reinfarction | 21.3 | 15.4 | 14.8 | .03 |
| Death | 22.5 | 24.3 | 27.2 | ns |
HDL, high-density lipoproteins; LDL, low-density lipoproteins; NS, not significant; PHIHD, personal history of ischemic heart disease.
All of the continuous variables are expressed as mean (standard deviation) and the categorical variables, as percentages.
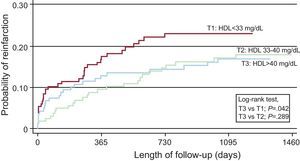
After a median follow-up of 4 years [interquartile range, 1-6 years], there had been 125 all-cause deaths (24.7%) and 87 reinfarctions (17.2%). The incidence of reinfarction was significantly higher in T1 (1.65/10 patients/year) and lower in T3 (0.99/10 patients year). In the multivariate analysis for competing events, after adjusting for variables related to risk of reinfarction (history, revascularization), potential confounding variables (age, history, Killip class on hospital admission, lymphocyte count, statin treatment, and LDL levels), and all-cause death as a competing adverse event, the patients in T1 had a significant increase in risk of reinfarction compared with those in T3 (hazard ratio=1.84; 95% confidence interval, 1.07-3.16; P=.028), as can also be seen in the Kaplan-Meier curve (Figure). The LDL and total cholesterol concentrations were not associated with the risk of reinfarction.
Kaplan-Meier curve estimating the probability of reinfarction over the long term. Multivariate analysis including the variables described in the text. HDL, high-density lipoproteins; T1, HDL level in the lowest tertile; T2, HDL level in the middle tertile; T3, HDL level in the highest tertile.
The major implications of our study are that, following ST-segment elevation acute coronary syndrome, the predictors of reinfarction over the long term in this consecutive, single-center population are very limited, and an HDL level in the lowest tertile is one of them. Our study is among the few that relate low HDL concentrations and the occurrence of a new infarction over the long term. In a subanalysis of the MIRACL (Myocardial Ischemia Reduction with Acute Cholesterol Lowering) trial,5 the low HDL levels observed during hospital stay were found to be related to the development of new clinical events after 16 weeks and, as in our study, these events were not influenced by LDL levels; it may be important to demonstrate the consistency of these results in a sample studied in a real life scenario and over a longer period of time.
Clinical practice guidelines6 consider low HDL concentrations to be a risk factor for cardiovascular events in primary prevention; however, they make no reference to the prognostic role in patients with cardiovascular disease, nor do they consider this to be a therapeutic objective. Our study adds a certain amount of consistency to the idea that this parameter should be taken into account in the integrated assessment of patients following acute coronary syndrome, until we can introduce effective tools to increase these levels and, thus, reduce risk.
.