Hemoperitoneum is a major cause of acute abdomen, and documented evidence suggests that pericardiocentesis is a possible underlying iatrogenic cause.
We present the case of a 76-year-old man who developed a hemoperitoneum and hypovolemic shock secondary to injury to the left inferior phrenic artery during echo-guided pericardiocentesis. Surgery was required to stop the bleeding.
The patient presented with exertional dyspnea, orthopnea, oligoanuria, and lower limb edema. The patient had a history of arterial hypertension, dyslipidemia, type 2 diabetes, obesity, peripheral vascular disease, diabetic retinopathy, chronic kidney disease, chronic obstructive pulmonary disease, intestinal angiodysplasia, and ischemic stroke treated with clopidogrel. Cardiopulmonary auscultation revealed arrhythmic and muted heart sounds with bibasal crackles. An electrocardiogram and blood enzyme analysis revealed no signs of myocardial ischemia, but did show a worsening of renal function parameters compared with previous readings. Suspected heart failure was assessed by echocardiography, which revealed severe pericardial effusion (26mm) with signs of hemodynamic deterioration. Echo-guided subxiphoid pericardiocentesis was performed, without attaching a drainage catheter, yielding a serous fluid with no atypical cells in the pathological analysis.
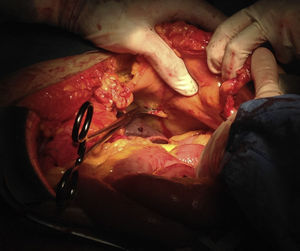
The patient made good clinical progress, but on the sixth day after the pericardiocentesis he developed sudden symptoms of hypotension and tachycardia that did not respond to volume infusion. A bedside examination by focused assessment with sonography in trauma (FAST) revealed abundant free intra-abdominal fluid, with limited pericardial effusion. Blood analysis showed a decrease in hemoglobin concentration from 11.7 d/dL to 5.5g/dL and a Quick index of 87%. Due to the hemodynamic instability, the decision was taken to perform an emergency laparotomy, revealing a 3200mL hemoperitoneum and a free flowing hemorrhage of the left inferior phrenic artery, with no other abdominal lesions. Bleeding was controlled by clamping (Figure) and hemostatic suture with 2/0 monofilament suture thread. During the intervention, the patient needed blood transfusion with 4 units of red blood cells, 1 platelet pool, and 3 units of fresh plasma. The patient made satisfactory clinical progress, returning to oral nutrition, recovering bowel transit, and showing improved cardiac function and a return to normal hemoglobin concentration. The patient was discharged from hospital 21 days after the intervention.
When associated with hemodynamic instability or serious injury to abdominal viscera, hemoperitoneum is a clinical situation that requires emergency surgery due to the associated high mortality.
The causes of hemoperitoneum can be divided into traumatic (open or closed abdominal trauma) and nontraumatic (coagulation disorders, gynecological illness, gastrointestinal perforation, spontaneous rupture of organs or neoplasms, pancreatitis, and vascular or idiopathic alterations). Cases of iatrogenic hemoperitoneum have been reported after percutaneous puncture for drainage of fluid collections, biopsy extraction, or thoracentesis or after procedures such as epicardial ablation of arrhythmias via the intrapericardial route1; however, there have been no previous reports of the need for laparotomy to stop the bleeding.
Complications secondary to pericardiocentesis are today rare (less than 4%) due to the use of ultrasonography, and the most frequently reported complications are arrhythmias, pneumothorax, and injury to the myocardium or coronary arteries. Less frequent complications are peritoneopericardial communication in peritoneal dialysis patients,2 pneumoperitoneum, hepatic or gastric puncture, and injury to the diaphragm or internal thoracic artery.3
Hemoperitoneum due to injury to the inferior phrenic artery has been documented in multiple trauma victims, patients with neoplasms or chronic pulmonary disease, and those undergoing thoracic surgery or toracentesis.4 In almost half of cases, the inferior phrenic arteries originatefrom the abdominal aorta, as a common branch or as independent arteries. In 45% of cases, they emerge from the celiac trunk, and in very rare cases they originate from other arteries, such as the left renal (5%), left gastric (2%), or hepatic artery (1%).5 Hemorrhage secondary to injury to these arteries is normally mild and self-limiting. Therefore, if the patient is hemodynamically stable, the recommended therapeutic measures are clinical observation and monitoring of analytical and imaging parameters. Other treatment options, such as embolization of the injured artery by interventional radiology techniques, might be indicated in hemodynamically stable patients with no other diaphragmatic or abdominal injuries.3 Otherwise, in patients showing signs of instability, a FAST examination is mandatory. This simple and reproducible test is conducted with a 3.5-MHz ultrasound probe at the patient's bedside and detects pericardial or pleural effusion and free abdominal fluid with high sensitivity and accuracy,6 providing an indication for emergency laparotomy in cases of suspected hemoperitoneum.