Brugada syndrome (BrS) is a hereditary arrhythmogenic disease characterized by a specific electrocardiographic pattern and a higher risk of sudden cardiac death due to ventricular tachyarrhythmias in patients with no structural heart disease1. The electrocardiographic pattern is dynamic and drug challenge to provoke a Brugada electrocardiographic pattern is an essential tool in the diagnosis of this syndrome2. Fever has been identified as a factor that can unmask the electrical pattern of BrS and trigger ventricular arrhythmias. The pathophysiological role of fever as an inductive mechanism in BrS has yet to be defined, but it is thought to be due to sodium channel inactivation secondary to body temperature in patients with mutations in the SCN5A gene3.
We report a case of electrical storm in a BrS patient triggered by the extremely high temperatures experienced during the record heat wave that occurred in Spain and other parts of Europe during the summer of 2015. The patient was a 34-year-old man who presented to the emergency department of a university hospital after an episode of syncope and repeated shocks from his implantable cardioverter-defibrillator (ICD).
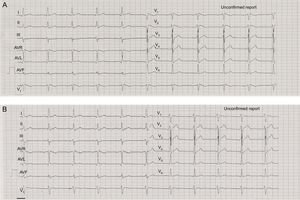
The patient had visited the emergency department 8 months earlier after experiencing a sudden loss of consciousness in a crowded discotheque. On arrival, the electrocardiogram (ECG) revealed the typical Brugada pattern with right bundle branch block morphology and ST-segment elevation in V1 and V2 (coved morphology). Echocardiography showed the heart to be structurally normal. He was diagnosed with BrS and underwent ICD implantation.
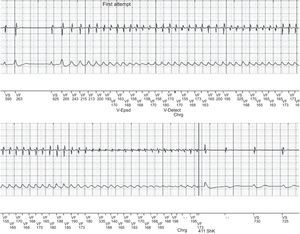
The patient experienced no new events until July 3, 2015. That afternoon, he was playing in a park with his 5-year-old son when the episode of syncope occurred and he received repeated shocks from the ICD. At that time, the thermometers were registering one of the highest temperatures of that summer, 42.7°C (108.86 °F). On admission, the patient was stable and the physical examination was normal, except for an axillary temperature of 37.5°C, with no signs or symptoms of infection. The ECG showed the typical Brugada pattern (Figure 1A). The results of the laboratory tests were normal (serum potassium, magnesium and calcium concentrations and inflammatory markers). Isoprenaline therapy was begun, and there were no new episodes of ventricular tachycardia or premature ventricular contractions, the patient's body temperature fell with no need for additional measures, and the ECG returned to normal within 24hours (Figure 1B). Device interrogation showed that all the parameters were normal. Four episodes of ventricular fibrillation were correctly detected, and shocks were delivered at 41 joules (Figure 2). After 3 days of observation, the patient was discharged with strict recommendations to avoid being outdoors during the hours of maximum heat and exposure to indoor settings with high temperatures and was given advice on the usual measures to prevent fever. After 9 months of follow-up, the patient remained asymptomatic and had reported no further events.
Several mutations in the SCN5A gene have been identified that encode for sodium channels in up to 20% to 30% of BrS patients. The genetic basis of this disease includes loss-of-function mutations in the genes encoding the cardiac sodium channels, which reduce the normal duration of the action potential. The effect is more pronounced in regions where the refractory periods are heterogeneous (with normal and mutated sodium channels), as occurs in the right ventricular epicardium. These differences lead to reentry circuits that result in the development of premature ventricular contractions and ventricular arrhythmias.
A number of conditions have been proposed as possible triggers of the Brugada electrocardiographic pattern, including fever, electrolyte disturbances, drugs, or medication (for example, cocaine, anesthetics, antiarrhythmic agents, antidepressants, and antihistaminic agents)3.
Fever is one of the factors most frequently reported to be a trigger of the Brugada electrocardiographic pattern, provoking episodes of ventricular tachyarrhythmia. In a large series of BrS patients, fever was the factor triggering the arrhythmias in 18% of the participants4. The hypothesis proposed to explain the causal mechanism of this triggering factor was temperature-dependent inactivation of the sodium channel in patients with the SCN5A mutation.
Moreover, the literature includes a few isolated cases of the unmasking of the Brugada electrocardiographic pattern by a heatstroke5,6. However, to date, there is absolutely no evidence of the triggering of ventricular arrhythmias in this setting.
In July 2015, a heat wave hit Spain and other European countries, with temperatures of over 40°C (104 °F). Our patient experienced ventricular arrhythmias on one of the hottest days in Spain, with temperatures of up to 42.7°C (108.86 F). This report illustrates a case in which the high outdoor temperatures may have contributed to sodium channel inactivation, triggering the Brugada electrocardiographic pattern and the recurrent episodes of ventricular fibrillation.