The incidence of primary cardiac tumors remains unknown. Figures vary widely depending on the series consulted (0.0017-0.19%),1–3 and data can be biased depending on the type of population cohort analyzed.
The aim of this study was to perform an epidemiological analysis of the age-adjusted incidence of cardiac myxoma (CM), the most common primary cardiac tumor, and to determine if there had been an increase in the number of cases diagnosed in our historical series spanning 30 years.
To establish the incidence of CM in our institution, we reviewed the pathology reports of samples sent from the cardiac surgery operating room between 1976 and 2016, in collaboration with the Epidemiology Division of the Department of Health of the Murcia region of Spain. An analysis was carried out of the age-adjusted incidence (AAI) of CM, using the world and European populations as references, and 2 historical periods were compared: 1990 to 2001 and 2002 to 2014. Cases diagnosed before 1990 were excluded because the records from before this date were not computerized. Survival analysis was performed with the Kaplan-Meier estimator (KM, log-rank test), and the cumulative incidence function was calculated using 1 – KM, censoring all competing events. A linear regression model was used to establish if there had been an increase in the number of diagnosed cases of CM, in 5-year periods. The statistical programs used were MedCalc 16.4.3 (MedCalc Software BVBA; Ostend, Belgium) and STATA 12 (StataCorp LP; College Station, Texas, USA).
Sixty-three patients were identified. The mean age at diagnosis was 57.3±13.7 years. Sixty-two percent (n=39) were women, and the female:male ratio was 1.25:1.
Adjusting to the world population as a reference, we obtained an AAI of 0.16 (95% confidence interval [95%CI], 0.11-0.20) per 100 000 population, and we found an increase when we compared the 2 historical periods 1990 to 2001 (n=14; AAI=0.08; 95%CI, 0.04-0.13) and 2002 to 2014 (n=38; AAI=0.23; 95%CI, 0.15-0.29). Adjusting to the European population, we obtained an AAI of 0.21 (95%CI, 0.15-0.26)/100 000; we also found an increase when comparing the periods 1990 to 2001 AAI=0.11; 95%CI, 0.05-0.17) and 2002 to 2014 (AAI=0.30; 95%CI, 0.21-0.38). Linear regression showed a significant increase in the number of cases of CM diagnosed in the last three 5-year periods of the series (β coefficient=0.84; 95%CI, 0.74-5.12; P=.019). The cumulative risk of CM until age 75 years was calculated at 0.02% for the period 2002 to 2014 (95%CI, 0.016-0.069) in the absence of competing risks of mortality.
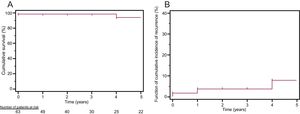
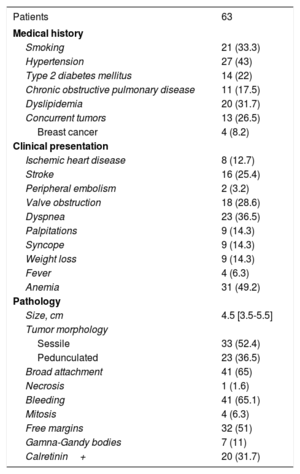
Table 1 shows the presence of cardiovascular risk factors and associated neoplasia, the clinical presentation, and the tumor pathology. Dyspnea was the most common clinical presentation, in 23 patients (36.5%), followed by stroke: 16 (25.4%) and ischemic heart disease: 8 (12.7%). In-hospital mortality was 3.20% (n=2). Five-year survival was 93.65%, with a median survival of 25.97 (95%CI, 23.69-28.25) years (Figure 1A). Over the whole period studied, 4 patients (6.35%) had tumor recurrence, 2 with Carney complex (3.1%) and 2 with isolated recurrence (3.1%); the median time to recurrence was 24.99 (95%CI, 22.13-27.85) years (Figure 1B).
Demographic, Clinical, and Pathological Variables
| Patients | 63 |
|---|---|
| Medical history | |
| Smoking | 21 (33.3) |
| Hypertension | 27 (43) |
| Type 2 diabetes mellitus | 14 (22) |
| Chronic obstructive pulmonary disease | 11 (17.5) |
| Dyslipidemia | 20 (31.7) |
| Concurrent tumors | 13 (26.5) |
| Breast cancer | 4 (8.2) |
| Clinical presentation | |
| Ischemic heart disease | 8 (12.7) |
| Stroke | 16 (25.4) |
| Peripheral embolism | 2 (3.2) |
| Valve obstruction | 18 (28.6) |
| Dyspnea | 23 (36.5) |
| Palpitations | 9 (14.3) |
| Syncope | 9 (14.3) |
| Weight loss | 9 (14.3) |
| Fever | 4 (6.3) |
| Anemia | 31 (49.2) |
| Pathology | |
| Size, cm | 4.5 [3.5-5.5] |
| Tumor morphology | |
| Sessile | 33 (52.4) |
| Pedunculated | 23 (36.5) |
| Broad attachment | 41 (65) |
| Necrosis | 1 (1.6) |
| Bleeding | 41 (65.1) |
| Mitosis | 4 (6.3) |
| Free margins | 32 (51) |
| Gamna-Gandy bodies | 7 (11) |
| Calretinin+ | 20 (31.7) |
Values are expressed as: No. (%) or median [interquartile range].
The most important contribution of our study to current knowledge of CM is that detection and diagnosis have increased in recent years, indicating a higher incidence. In 2011, Sigurjonsson et al.4 carried out the first epidemiological study of the AAI of CM, and found an incidence of 0.11 cases/100 000 population. Our AAI of 0.16 along with the increase when comparing the 2 historical periods indicates an underdiagnosis in previous decades (assuming an incidence lower than the real incidence) and the crucial role played by the development of cardiac imaging techniques for the differential diagnosis of cardiac masses.5 Increased accessibility to echocardiography and professional specialization in the field could explain this marked increase in the number of cases of CM diagnosed per year, bearing in mind that changes in the use of the diagnostic techniques and in the organizational structure of the facility could have influenced the estimates performed and the incidence data obtained.
The additional findings of our study relate to the clinical behavior of CM. In 25% of the patients, the clinical presentation was stroke. This confirms CM as a cause that should be included in the differential diagnosis of ischemic stroke in patients in the fifth decade of life, and a reason for performing more exhaustive imaging tests in cases of stroke of unknown origin (approximately 1/3 of diagnosed strokes in patients aged 45 to 64 years).6 Few studies have looked at the coexistence of other tumor types in patients with CM.1,3 In our series, 26.5% of the patients had a second diagnosis of a different tumor in a different location, the most frequent being breast cancer. This high incidence highlights the need to perform additional investigations at the time of CM diagnosis to look for other concurrent cancers and open avenues of clinical research into the etiology and natural history of this type of tumor.
In conclusion, the most precise data on CM incidence show an increase in the diagnosis of these tumors in recent years and demonstrate the essential role of echocardiography.