To the Editor,
We present the case of a 58 year-old woman with dyslipidemia, an ex-smoker, with no known history of heart problems, diagnosed with oat-cell lung carcinoma two years earlier. She experienced extreme fatigue and inability to make fine movements for 10 days and sought emergency care. A cerebral computed tomography (CT) revealed a space-occupying lesion in the right frontal region, indicative of metastasis. A CT of the chest, abdomen, and pelvis did not show any relevant findings. We started the patient on high doses of corticosteroids and presented the case to the brain tumor committee, which opted for excision of the lesion. The patient underwent a preoperative electrocardiogram (ECG) (Figure 1) and scheduled surgery on a week later. During anesthetic induction, the patient had increased blood pressure with alterations in the ECG, suggesting subepicardial ischemia (Figure 2). The procedure was halted and the cardiology department was consulted. An echocardiogram did not reveal any segmental changes in contractility or associated valvulopathies; and left ventricular ejection fraction was preserved. Markers of myocardial damage were not elevated. However, given the possibility of non ST-segment elevation acute coronary syndrome and the need for a definitive diagnosis, it was performed a coronary angiography. We did not observe any significant lesions in the angiography. The patient was discharged from cardiology with the same electrocardiographic alterations. Sixteen days after discharge, she was readmitted to neurosurgery, the preoperative ECG had normalized. A right frontoparietal craniotomy was performed with radical excision of the space-occupying lesion, using the same anesthetic induction as before, but this time without incident.
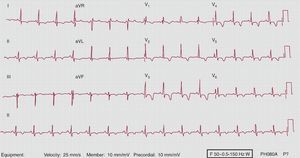
Figure 1. Preoperative electrocardiogram.
Figure 2. Electrocardiogram during anaesthetic induction, showing diffuse and deeply inverted T-waves.
ECG is a useful diagnostic tool based on the recording of electrical activity in the heart. A differential diagnosis of acute T-wave changes can be time-consuming and complicated, and can include hydro-electrolytic alterations (especially hypocalcaemia and hyperkalemia), hypothermia, pulmonary embolism, cardiovascular disease, and central nervous system (CNS) disorders, among others.
The association of electrocardiographic abnormalities with intracranial damage has been known for decades. Burch et al.1 were the first to described its association with acute cerebrovascular accidents (ACVA). These electrocardiographic changes can occur in patients with a previously normal electrocardiographic readout, and they can occur at any age, even adolescence. Although the majority appear in ACVA, can also occur in ischemic ACVA and non-vascular intracranial lesions.2, 3 Electrocardiographic anomalies can be found in 42% of patients with tumors of the brainstem and 56% with intracerebral tumours.4
Disorders of the CNS usually cause abnormalities in ventricular repolarisation. The most common findings are: elevated or depressed ST-segment, inverted T-waves, prolonged QT interval–the most common–and presence of U-waves.3 These alterations can be transient or may remain for several weeks. The electrocardiographic changes observed in Figure 2 often occur in ACVA although they have also been described in Stokes-Adams attacks and intracranial tumours.4
The pathophysiology of this entity is still unclear. Several different mechanisms have been proposed, including elevated intracranial pressure, vagal tonicity, and excessive stimulation of the sympathetic nervous system with catecholamine production. The predominating theory involves the neurohormonal system. Damage to the CNS can result in increased catecholamine levels and sympathetic outflow, which would not only cause electrical problems, but also could lead to physical myocardial damage.5 Catecholamines probably have a direct toxic effect on myocardial cells or mediate a vasoconstrictive effect on the coronaries.
Complications may arise during anaesthetic due to the cardiovascular depression caused by the anesthetic agents. In our case, we used: propofol, midazolam, and fentanyl, using the appropriate doses based on body weight. In this context, the potential side effect would be transient arterial hypotension. Benzodiazepines have mild hemodynamic effects, and as regards opioids, fentanyl produces no changes in myocardial contractility. With this in mind, the most probable effect of the anaesthetic in this context is transient arterial hypotension, which did not occur in our case; nor did we observe signs of hemodynamic instability. As such, we can rule out a relationship between the electrocardiographic changes and the anesthetic induction used; we consider that this finding was related to the neurological process occurred in the perioperative context. Abnormalities exclusive to T-waves are not diagnostic of any condition in particular. T-waves must be evaluated together with QRS complex, ST-segment, and clinical conditions of the patient. In this case, anamnesis was not possible, and in light of the suspicion of coronary disease and the need for a definitive diagnosis, we performed a coronary angiography.
Cardiac and neurological diseases frequently overlap.6 The electrocardiographic changes that are associated with alterations in the CNS have both theoretical and practical importance, since in many occasions they may seem to be heart disease and can lead to an incorrect diagnosis, with therapeutic and prognostic implications.
As such, non-cardiac causes, including alterations of the CNS, should be considered in the differential diagnosis of diseases resulting in ECG changes, especially when the clinical history does not suggest acute coronary syndrome.
Corresponding author: mtl.lluva@gmail.com