Heart rate (HR) is a parameter with prognostic value in patients with heart failure (HF), reduced ejection fraction and sinus rhythm, showing an inverse relationship with cardiovascular outcomes.1 The ESC Heart Failure guidelines2,3 included the achievement of a HR <70 bpm and a specific drug for HR slowing (ivabradine) in their treatment algorithm.
This indication is based on the SHIFT study4 (stable chronic HF patients). However, in our recently published ETHIC-AHF study,5 we demonstrated the safety and efficacy of early coadministration of ivabradine and beta-blockers (Iv+BB) during hospitalization in patients with acute systolic HF and sinus rhythm. There are no other randomized data on ivabradine use in acute HF.
The ETHIC-AHF study, whose protocol and results at 4 months have been recently published,5 compared the strategy recommended by guidelines vs that of early simultaneous administration of Iv+BB. The objective of the present study was to analyze the effect of this strategy on the long-term follow-up of these patients. Events during follow-up were analyzed by the Kaplan-Meier method and a Cox regression method was used for time to first event comparison. Analyses were adjusted for baseline HR.
Between November 2013 and April 2015, 71 patients were randomized: 33 to the intervention and 38 to the control group. Both groups were homogeneous in age, sex, blood pressure, HR, B-type natriuretic peptide levels and treatment at discharge. Patients in the intervention group had lower HR at 28 days and 4 months of discharge, greater left ventricular ejection fraction, lower B-type natriuretic peptide levels, and a trend to better functional class.
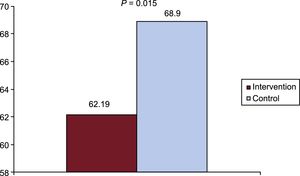
After a mean follow-up of 27±11 months, patients randomized to the intervention group continued to have lower HR (62.19±7.8 bpm vs 68.9±10.5 bpm; P=.015, Figure 1). The proportion of patients taking BB was similar in both groups (94.7% vs 88.9%; P=.49), as was the percentage of patients receiving medium-high doses (> 5mg/d of bisoprolol or >25mg/d of carvedilol), 38.9% vs 54.2%; P=.56. Mean dosages of bisoprolol and carvedilol were similar in both groups during follow-up. For bisoprolol: 3.8±0.3 vs 3.9±0.3mg/d at discharge; 6.7±0,9 vs 7.6±0.7mg/d at 4 months; 7.5±0.7 vs 7.6±0.7mg/d at 1 year; and 7.4±0.6 vs 7.5±0.6mg/d at the end of follow-up (intervention vs control groups). For carvedilol: 8.4±1.2 vs 9.1±1.3mg/d at discharge; 20.3±4.6 vs 27.8±4.8 at 4 months; 25.2±4.9 vs 28.6±4.7 at 1 year: and 26.6±5.1 vs 27.7±4.8mg/d at the end of follow-up. The proportion of patients taking ivabradine was also similar in both groups (68.4% vs 42.9%; P=.085), although more patients were receiving 7.5mg/12h in intervention group (84.6% vs 10%; P <.001).
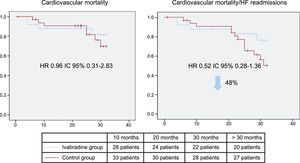
Left ventricular ejection fraction was higher in the intervention group at 4 (44.8±14.4 vs 38.1±6.1%; P=.039), 12 (48.2±17 vs 41.8±10%; P=.002), and 32 months (48.5±15 vs 42±12%; P=.1). When we analyzed the incidence of major cardiovascular events, patients in the intervention group showed a trend to having lower rates of HF readmissions (18.8 vs 28.2%; P=.1), and a lower rate of the combined endpoint of HF readmissions and cardiovascular mortality (hazard ratio=0.52; 95% confidence interval, 0.28-1.36; P=.1; Figure 2). In absolute numbers, 7 vs 13 patients had an event (HF readmission and/or mortality due to cardiovascular causes) beyond 4 months of follow-up. After a mean follow-up of 27 months, there were no severe drug-related adverse events.
These results show that early addition of Iv+BB in this context is safe in the short-term5,6 and that there was a potential prognostic benefit of this strategy in the long-term, since patients randomized to the Iv+BB strategy showed better HR control as early as 28 days after discharge, and a significant difference persisted in the long-term follow-up, despite the recommended up-titration of BB in both groups of patients. This was associated with a trend to lower HF readmissions and cardiovascular mortality rates. These results could not be reasonably attributed to differences in BB use, since the proportion of patients taking BB and other drugs was similar in both groups, as were the doses of these drugs.
We conclude that long-term follow-up analysis of the ETHIC-AHF study shows that early coadministration of Iv+BB during hospitalization due to acute systolic HF is feasible and safe, and permits better HR control from earlier stages after discharge, showing a trend to improve prognosis.