Keywords
INTRODUCTION
Myocardial changes caused by diabetes mellitus (DM) in the absence of ischemic heart disease (IHD), high blood pressure or other known causes of cardiopathy are known as diabetic cardiomyopathy. Diastolic dysfunction of the left ventricle (DDLV) is thought to be the first functional abnormality. Structural changes such as a thickening of the myocardium of the left ventricular mass have also been described. An increase in the ventricular volumes and anomalies in contractility may finally appear.1
Some studies with small numbers of patients have indicated that, compared to non-diabetics, the concentration of NT-proBNP is increased in patients with type 2 diabetes only when this is accompanied by microvascular and/ or macrovascular complications.2 Given the physiopathology of diabetic cardiomyopathy and the stimuli that induce the synthesis and secretion of NT-proBNP, it is possible that echocardiographic abnormalities might be appreciable and that the levels of this peptide are increased in patients with DM, even when the latter is not accompanied by vascular complications. The present study, which has a larger number of patients than any of its forerunners, examines this hypothesis. The aims of this work were therefore to detect any echocardiographic differences, and any differences in the NT-proBNP concentration, between a control group and groups of patients with DM with and without IHD, and to determine whether NT-proBNP could be used as a diagnostic marker of IHD in diabetics.
METHODS
Study Population
The study subjects were 284 patients over 30 years of age who, between March 2004 and August 2005, presented at our cardiology clinic for reasons of primary prevention or for annual check-up of their IHD. These patients were divided into 3 groups: 99 with neither DM nor IHD (control, group 1), 110 with type 2 diabetes but with no IHD (group 2), and 75 with type 2 diabetes plus IHD (group 3).
Any subject with DM or any carbohydrate metabolic abnormality (detected via a glycemia curve) was excluded from group 1. Type 2 diabetes was diagnosed using the criteria proposed by the American Diabetes Association.3 The patients in groups 2 and 3 were selected depending on their known background of IHD or documented ischemia in tests following current recommendations.4 Patients with a left ventricular ejection fraction of <45% were excluded from the study, as were all those suffering heart disease of non-ischemic origin.
Echocardiographic Study
All patients were examined by the same echocardiographer using a Sonos HP 5500 apparatus with a 3 MHz probe with a second harmonic and software for tissue Doppler examination. A morphological study of the left ventricle was undertaken. The ejection fraction was estimated according to the method of Teichholz, and the shortening fraction and mesocardial shortening fraction calculated according to the formula of Simone.5 The study of the diastolic function included analysis of the transmitral flow and the propagation velocity, and tissue Doppler analysis of the mitral ring. Mitral filling patterns were established according to the criteria of Khouri et al6 and García et al.7
Determination of NT-proBNP
Plasma NT-proBNP was determined using a commercial ELISA kit, employing an anti-serum specific to the amin-terminal (Biomedica Gruppe, Germany).
The inter- and intra-analytical coefficients of variation were 4% and 5%, respectively. Sensitivity was 5 fmol/mL.
Statistical analysis
The cross-sectional, descriptive and comparative analysis of the quantitative and qualitative variables involved the c2 test or ANOVA with a post-hoc Bonferroni test. Quantitative variables were expressed as means (standard deviations); categorical variables were expressed as percentages. Significance was set at P<.05. The usefulness of NT-proBNP as a marker of ischemia was determined by ROC curve analysis. All calculations were performed using SPSS® v. 11.0 software (SPSS Inc.).
RESULTS
Table 1 shows the clinical characteristics of the patients.
Analysis of the Form and Systolic Function of the Left Ventricle
Table 1 shows the structural differences detected. The shortening fraction was significantly smaller in the group 3 patients than in those of group 1. No differences were observed in terms of systolic function.
Analysis of Diastolic Function
Compared to the control group, both groups of diabetic patients contained a greater proportion of subjects with DDLV (group 1, 74%, group 2, 88%, group 3, 90%; P<.001; no significant difference between the groups of diabetic patients) (Table 2). The percentage atrial contribution to ventricular filling, estimated via automatic edge detection, was significantly greater in group 2 than group 1 subjects (Table 1).
Plasma NT-proBNP Concentrations
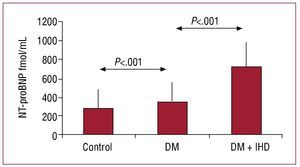
The NT-proBNP concentration increased from group 1 to group 3, with significant differences in all comparisons (281.7 [190.4], 350.6 [197.8], and 720.6 [278.1] fmol/mL respectively; P<.001) (Figure 1). No correlation was seen between NT-proBNP concentration and the different variables or stages of DDLV.
Figure 1.Concentrations of NT-proBNP in the three groups.
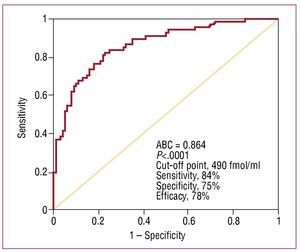
The usefulness of NT-proBNP as a marker of IHD in patients with type 2 diabetes was assessed by ROC curve analysis. The area under the curve was 0.864 (0.029) (P<.0001) (Figure 2). A concentration of >490 fmol/mL showed 84% sensitivity and 75% specificity for a diagnosis of IHD, with a RR of 15.1 (95% CI, 7.07-34.2; c2=56.05; P<.0001).
Figure 2. ROC curve for NT-proBNP for distinguishing between the patients with diabetes and ischemic heart disease.
DISCUSSION
In this study, the diabetic patients without IHD showed DDLV more frequently and had higher NT-proBNP concentrations than controls of the same age. In the group of patients with IHD, the plasma NT-proBNP concentration was much higher than in the other two groups. Many reports indicate DDLV to be very common among asymptomatic diabetics, and anomalies in ventricular filling have been detected in up to 75% of patients with diabetes.8 The results of the present study resemble these figures. The mean age and prevalence of high blood pressure in the patients of the control group explain the high prevalence of DDLV among them.
It has been indicated that an elevated BNP concentration in diabetic subjects is associated with hypertrophy of the left ventricle and systolic and diastolic dysfunction; it could therefore be a prognostic factor for morbidity/mortality.9 In the present work, although DDLV and higher NT-proBNP concentrations were found in the diabetic patients without IHD (compared to the control group), no correlation was seen between elevated NT-proBNP and the degree of diastolic dysfunction.
B-type natriuretic peptide and NT-proBNP are of great prognostic value in stable and unstable angina, and in acute myocardial infarction.10 In the present study, the subjects with type 2 diabetes plus IHD were all stable, asymptomatic patients who came to the clinic for a check-up. In these patients the concentration of NT-proBNP was much greater than in those with type 2 diabetes but no IHD, indicating that this peptide could be a useful biochemical marker in the diagnosis of IHD in diabetics. This interesting possibility needs to be confirmed in further studies. It should be remembered that the patients in this study represent quite well the spectrum of patients in whom the determination of the NT-proBNP concentration would be of use, ie, patients that come to clinics for tests to rule out IHD. As seen in the present work, high NT-proBNP concentrations in these patients could be an indication of the risk of IHD.
Limitations
Several factors influence the plasma concentration of NT-proBNP,11 especially sex and obesity, and these variables were not equally distributed in the present groups. Since women have higher NT-proBNP concentrations than men, and since those of obese people are lower than those of the non-obese, the present composition of the groups may have hidden differences between them-but in the same direction of those actually found. Hypercholesterolemia and the use of tobacco were also unequally distributed in the present groups, but it is not known whether these factors influence the NT-proBNP concentration. It should also be remembered that ischemia detection tests are not 100% sensitive; thus, it cannot be ruled out that some patient in the DM without IHD group actually had IHD although the necessary tests were performed when indicated. In the group of patients with DM plus IHD, although an ejection fraction of >45% was required for inclusion (as in the other groups) the actual degree of ischemia was not quantified. Finally, the estimation of the ejection fraction by the Teichholz method has known limitations.
In conclusion, the patients with DM but without IHD more often had DDLV and showed an increased NT-proBNP concentration in the absence of structural differences or differences in systolic function compared to the control group. The NT-proBNP concentration was even higher in the patients with DM plus IHD. A concentration of 490 pg/mL is associated with high sensitivity and specificity in the detection of IHD in patients with DM.
Full English text available from: www.revespcardiol.org
Correspondence: Dra. S. Castaño.
Departamento de Cardiología. Clínica Universitaria de Navarra. Avda. Pío XII, 36. 31008 Pamplona. Navarra. España.
E-mail: scastano@unav.es
Received November 3, 2008.
Accepted for publication January 28, 2009.