Patient sedation is a fundamental aspect of catheter ablation procedures. In prolonged or painful procedures, such as atrial fibrillation (AF) ablation, the patient may receive “conscious sedation”, which does not prevent involuntary movements or perception of pain, or general anesthetic.1 The choice of one or the other depends on patient characteristics and anesthetist availability. “Deep sedation” with propofol has been developed as a third alternative in AF catheter ablation.1–4 This option can achieve immobility and complete analgesia without the need for intubation or general anesthetic. We describe our experience with this technique.
We prospectively included all patients who underwent AF ablation in our hospital from July 2012 to December 2016. The study was authorized by the local ethics committee. The ablation procedure has previously been described elsewhere.5 Briefly, via the right femoral vein, we introduced 1 decapolar catheter up to the coronary sinus, and, via a single transseptal puncture, one 3.5 mm irrigated ablation catheter and 1 circular mapping catheter. Patients were anticoagulated with heparin sodium to maintain an activated clotting time of between 250 and 350seconds. With a CARTO3 navigation system (Biosense Webster), antral ablation of ipsilateral pulmonary vein pairs was performed; radiofrequency was delivered at 35/25W at 45°, and irrigation at 30/17mL/min. The aim of ablation was bidirectional block of the pulmonary veins. A nurse administered the “sedation protocol” (Table 1) under the supervision and instruction of the electrophysiologists. The airway was maintained patent with a Guedel airway and continuous oxygen therapy at 2 L/min via nasal prongs. Patient eye protection was with passive eyelid closure, held closed with surgical paper tape. In all patients, invasive arterial pressure, heart rate, and oxygen saturation were recorded every 15minutes throughout the procedure. The “procedure time” was taken as the time from femoral puncture until catheter withdrawal; “sedation time” was from the start of midazolam administration until the end of propofol administration, which was continuous until the activated clotting time was < 250seconds for the removal of the safety introducers; and “recovery time” was from the end of propofol administration until patients were fit to leave the electrophysiology laboratory to go to their room (conscious and hemodynamically stable). The day after the procedure, patients were given a questionnaire to evaluate the perception of pain and whether they would repeat the same type of sedation in the future, both variables being considered as dichotomous qualitative variables with 2 possible responses (yes/no).
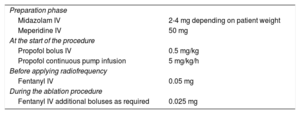
Sedation Protocol
| Preparation phase | |
| Midazolam IV | 2-4 mg depending on patient weight |
| Meperidine IV | 50 mg |
| At the start of the procedure | |
| Propofol bolus IV | 0.5 mg/kg |
| Propofol continuous pump infusion | 5 mg/kg/h |
| Before applying radiofrequency | |
| Fentanyl IV | 0.05 mg |
| During the ablation procedure | |
| Fentanyl IV additional boluses as required | 0.025 mg |
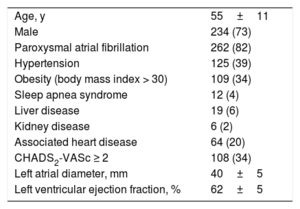
During the inclusion period, 320 AF ablation procedures were performed. The patients’ baseline clinical characteristics are shown in Table 2. The procedure time was 120±20minutes, and the aim was achieved in all patients. There was 1 major complication, a cardiac tamponade, which was successfully drained, and 2 pseudoaneurysms at the puncture site, which resolved with conservative management. Sedation time was 140±19minutes and recovery time was 20±5minutes. Six patients (1.9%) had hypoxemia (oxygen saturation < 90% for more than 20seconds) requiring manual ventilatory support with a bag valve mask for less than 2minutes. The other instances of hypoxemia were mild and resolved rapidly with a jaw thrust and temporary reduction in propofol infusion. Forty-five patients (14%) had hypotension (systolic arterial pressure < 90 mmHg for more than 3minutes), which responded to fluids and adjustment of the propofol infusion. No cases required CARTO3 map reconstruction due to patient involuntary movements. All patients went to a normal hospital ward once the procedure was finished, none reported pain or discomfort during the intervention, and all stated that they would opt for this type of sedation in the future.
Baseline Patient Clinical Characteristics
| Age, y | 55±11 |
| Male | 234 (73) |
| Paroxysmal atrial fibrillation | 262 (82) |
| Hypertension | 125 (39) |
| Obesity (body mass index > 30) | 109 (34) |
| Sleep apnea syndrome | 12 (4) |
| Liver disease | 19 (6) |
| Kidney disease | 6 (2) |
| Associated heart disease | 64 (20) |
| CHADS2-VASc ≥ 2 | 108 (34) |
| Left atrial diameter, mm | 40±5 |
| Left ventricular ejection fraction, % | 62±5 |
Values are expressed as No. (%) or mean±standard deviation.
Our data demonstrate that for patients undergoing AF ablation, deep sedation with propofol supervised by an electrophysiologist is effective (there are no involuntary patient movements and it avoids pain) and safe (no serious adverse events) and allows the procedure to be performed without the need for general anesthetic. This method of sedation could be very useful in centers without anesthetists and avoids preoperative anesthetic assessment and transfers to the recovery room. Future studies will tell if new drugs, such as dexmedetomidine, used in conscious sedation could be a valid alternative to this type of deep sedation.6 Since the patient population of this study was selected and relatively young, as happens in AF ablation, the results should not be extrapolated to older patients with advanced heart disease.
.