On February 2020, the coronavirus disease of 2019 (COVID-19) rapidly spread throughout Europe. Due to the lack of pharmacological treatment or vaccine, governments adopted measures called social distancing to reduce the peak intensity of the epidemic. In Spain, the government issued a decree declaring a state of alarm on 14 March, 2020.
Timely reperfusion therapy by primary percutaneous coronary intervention (pPCI) is recommended for patients with ST-segment elevation myocardial infarction (STEMI)1 and its benefit is time-dependent, with longer delays associated with worse outcomes. A recent survey of Spanish STEMI networks reported a reduction in pPCI procedures during the COVID-19 pandemic.2 We aimed to assess the reduction in STEMI admissions and changes in patient characteristics, delay times and early mortality during the first weeks of the COVID-19 pandemic in Catalonia.
In Catalonia, a Spanish region with 7.6 million inhabitants, acute care for patients with STEMI is organized through a regional network of 10 pPCI hospitals.
The AMI code registry collects data from all attended STEMI patients. The registry belongs to the health department of the Catalan government and its completion is compulsory and periodically audited. The database conforms to ethical and legal requirements for research purposes, and all study procedures are conducted in accordance with the ethical standards of the Helsinki Declaration.
All patients with a confirmed STEMI from 1 March to 19 April, 2020, were compared with patients attended within the same dates in 2019.
Delay times were defined according to the European Guidelines.1 Patient delay was defined as time from symptom onset to first medical contact. System delay as time from first contact to reperfusion therapy. Ischemia time as time from symptom onset to reperfusion therapy. Delay times were stratified by site of first medical contact.
Admission rates were estimated with Poisson regression models with time (days) as a continuous variable. Categorical variables are expressed as number and percentage and were compared with the chi-square test. Continuous variables are expressed as mean ± standard deviation and were compared with the Student t test. Time intervals are expressed as median [interquartile range] and were compared with the Kruskal-Wallis equality-of-populations rank test. Mortality at 10 days after activation was estimated for all patients with available information about vital status (STEMI occurring between March 1 and April 10).
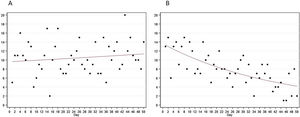
A total of 395 STEMI patients were admitted during the 2020 period and 524 during the same period in 2019. The mean number of daily admissions was 10.5 in 2019 and 7.9 in 2020 (incidence rate ratio, 0.75; 95% confidence interval, 0.66-0.86). In 2020, there was a significant 52% reduction in daily admissions from day 1 to day 50 (figure 1). There were few differences between the groups (table 1).
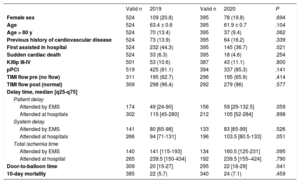
Characteristics, delay times and outcomes of patients with confirmed ST-segment elevation acute myocardial infarction
| Valid n | 2019 | Valid n | 2020 | P | |
|---|---|---|---|---|---|
| Female sex | 524 | 109 (20.8) | 395 | 78 (19.8) | .694 |
| Age | 524 | 63.4 ± 0.6 | 395 | 61.9 ± 0.7 | .104 |
| Age > 80 y | 524 | 70 (13.4) | 395 | 37 (9.4) | .062 |
| Previous history of cardiovascular disease | 524 | 73 (13.9) | 395 | 64 (16.2) | .339 |
| First assisted in hospital | 524 | 232 (44.3) | 395 | 145 (36.7) | .021 |
| Sudden cardiac death | 524 | 33 (6.3) | 395 | 18 (4.6) | .254 |
| Killip III-IV | 501 | 53 (10.6) | 387 | 43 (11.1) | .800 |
| pPCI | 519 | 425 (81.1) | 394 | 337 (85.3) | .141 |
| TIMI flow pre (no flow) | 311 | 195 (62.7) | 296 | 195 (65.9) | .414 |
| TIMI flow post (normal) | 309 | 298 (96.4) | 292 | 279 (96) | .577 |
| Delay time, median [q25-q75] | |||||
| Patient delay | |||||
| Attended by EMS | 174 | 49 [24-90] | 156 | 59 [29-132.5] | .059 |
| Attended at hospitals | 302 | 115 [45-280] | 212 | 105 [52-284] | .898 |
| System delay | |||||
| Attended by EMS | 141 | 80 [65-98] | 133 | 83 [65-99] | .526 |
| Attended at hospitals | 266 | 94 [71-131] | 196 | 103.5 [80.5-133] | .051 |
| Total ischemia time | |||||
| Attended by EMS | 140 | 141 [115-193] | 134 | 160.5 [125-231] | .095 |
| Attended at hospital | 265 | 239.5 [150-434] | 192 | 239.5 [155–424] | .790 |
| Door-to-balloon time | 309 | 20 [15-27] | 295 | 22 [18-29] | .041 |
| 10-day mortality | 385 | 22 (5.7) | 340 | 24 (7.1) | .459 |
EMS, emergency medical system; pPCI, primary percutaneous coronary intervention; TIMI, Thrombolysis in Myocardial Infarction.
Data are expressed as No. (%), mean ± standard deviation or median [interquartile range].
A similar reduction in STEMI admissions has already been reported in other settings.3–5 To our knowledge, this is the first study performed in Spain using individual patient data from a regional STEMI network. We observed a 50% reduction in STEMI admissions in 50 days and only slight differences in patient characteristics and delay times compared with patients admitted during the same period in 2019. Potential causes of this decrease in STEMI admissions include avoidance of medical care due to social distancing, STEMI underdiagnosis, and competing risk with the acquisition and severity of COVID-19, and warrant further investigation.
To all Codi IAM investigators: Josepa Mauri Ferré, Cardiología Hospital Universitari Germans Trias i Pujol, Pla Director de les Malalties Cardiovasculars, Departament de Salut, Generalitat de Catalunya; María Teresa Faixedas, Catsalut; Albert Ariza Sole, Hospital Universitari de Bellvitge – IDIBELL; Xavier Carrillo Suárez, Hospital Universitari Germans Trias i Pujol; Joan García Picart, Hospital de la Santa Creu i de Sant Pau; Rosa María Lidón Corbi, Hospital Universitari Vall d’Hebron; Sergio Giovanny Rojas Lievano, Hospital Joan XXIII de Tarragona; Ander Regueiro, Hospital Clínic de Barcelona; Helena Tizón, Hospital del Mar. To Josep Ramon Marsal for statistical advice.