Tricuspid regurgitation (TR) is classified as either primary or secondary according to the underlying mechanism. Moderate/severe TR has been associated with greater mortality than mild insufficiency, even in the absence of pulmonary hypertension or right ventricular dysfunction.1 Nevertheless, less than 18% of patients with severe TR are referred to tricuspid valve surgery.2 In the current era, technology has brought us the opportunity to treat those deemed at high risk for surgical valve replacement with the development of various tricuspid transcatheter valve interventions.3 We aimed to appraise the current management of TR ≥ 2+in our center, with special attention to the safety and feasibility bicaval valve implantation (CAVI).
In the first semester of 2018, of 3620 consecutive patients who underwent transthoracic echocardiography, a total of 97 (2.7%) had TR ≥ 2+and were followed up for 1 year to determine their outcomes. Of these, TR was severe in 41.7%, massive in 17.7%, and torrential in 2.1%.4 Mean age was 75.9±11.2 years, 65% were women and the most common etiology was secondary TR. Echocardiography determined a mean size of the tricuspid annulus (4 chambers) of 48.3±9.3mm, with an estimated tricuspid annular plane systolic excursion of 16.9±4.2 mm. Mean pulmonary artery systolic pressure was 53.6±14mmHg and left ventricular ejection fraction was 54.2±13.3%. At a mean follow-up of 323.9±101.4 days, 37.1% of the patients required hospital admission mainly due to heart failure (HF) (58.3%) and at least 7% had multiple readmissions. Overall, the most common strategy was medical treatment (93.8%) and 13 patients (13.5%) died mostly because of refractory HF (61.5%). Two patients underwent uneventful surgical repair with improvement but there was 1 periprocedural death due to right ventricular failure. One more patient, with suitable anatomy for edge-to-edge repair and lack of retrograde large V wave in the caval veins, underwent MitraClip (Abbott Vascular, United States) implantation in the tricuspid position without any clear improvement as a result of residual unchanged TR, despite immediate procedural success. Finally, 2 patients underwent CAVI as compassionate therapy after approval by competent authorities, including Tricento (NVT, Germany) and the first reported case in Spain with TricValve (Products&Features, Austria) systems.
The first CAVI case was a 58-year woman with a mitral mechanical prosthesis (Carbomedics n.25 valve. LivaNova, United Kingdom) implanted 11 years earlier, functional TR, dyspnea in New York Heart Association (NYHA) class III-IV, and multiple admissions due to HF. Transthoracic echocardiography showed massive TR due to secondary impaired coaptation of the leaflets because of right ventricular dilation with preserved function (51% according to magnetic resonance). After discussion by the Heart Team, it was decided to perform percutaneous implantation of Tricento. The patient was discharged 24hours after a successful procedure and at 30 days showed NYHA class I, improvement in the 6-minute walk test (6-MWT) from 408 to 475 meters, and reduction in TR to grade 2+.
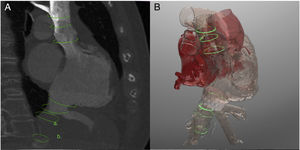
The second CAVI case was a 74-year woman who had undergone surgical mitral (Carbomedics n.25) and aortic (ATS n.18, Medtronic, United States) valve replacement 8 months previously. At that time, TR was moderate and there was no annular dilation, but after surgery severe TR developed leading to several readmissions due to decompensated right-HF with progression to massive TR. Therefore, the Heart Team decided to implant compassionate TricValve. Transfemoral venous approach implantation of the device was performed under transesophageal echocardiography, and hemodynamic evaluation demonstrated an abolished V wave in both the superior and inferior vena cava (figure 1). The patient was discharged 3 days later after blood transfusion due to pre-existing anemia. At 30 days, functional status improved to NYHA class II, 6-MWT from 158 to 239 meters, and TR persisted as severe but with reduction of pulmonary artery systolic pressure from 68 to 49mmHg.
A: computed tomography assessment of superior (20 x 25mm) and inferior vena cava (26 x 30mm). B: three-dimensional-biomodeling simulation of TricValve implantation based on computed tomography. C: superior vena cava prostheses. D: release of inferior vena cava prostheses. E, F: pre- (green) and post-TricValve (orange) implantation pressure curves. Baseline atrial curve shows a ventricularized sharp V wave (21mmHg) and post-TricValve shows an abolished V wave (12mmHg).
In general, the CAVI systems try to abate the backward blood flow into the caval veins,5 which are usually dilated at end-stage TR for damping HF symptoms. Its indication requires careful hemodynamic assessment (retrograde V wave and wedge pressure) and its correlation with the etiology of the dyspnea. Compared with orthotopic valves, there is a lower risk of cardiac injury or acute right ventricular failure; nevertheless, atrial and ventricular volume overload status remains because the structure of the native valve is not modified. The question of whether further dilation of the caval system might occur causing periprosthetic leakage and minimizing the clinical positive impact of this heterotopic strategy remains unanswered, but this initial experience reflects positive remodeling in the right heart and venous system in the short-term. Interestingly, the TricValve system offers standardized sizes and less interplay with the atrium as opposed to the Tricento device, which requires customize sizing. In addition, TricValve can be implanted in patients with a short distance from the inferior vena cava to the suprahepatic veins (< 10mm) because the sealed segment is shorter than with Tricento.5
In summary, TR is associated with high mortality in the short-term with medical treatment. Assessment of potential prognostic benefit by bicavally implanted heterotopic prosthesis requires longer term studies, but our initial experience suggests safe and effective procedural and short-term outcomes.
FundingThe institution received non-conditioned support due to its participation in the Tricus Study Euro.