Aortic stenosis (AS) is the most common valve disease in the elderly. Older patients may have suboptimal results with surgical or transcatheter (TAVI) aortic valve replacement,1 with higher rates of morbidity, mortality, and readmission, as well as worse quality of life, all of which stem from the particular characteristics of the disease in the elderly.2 Following the PARTER3 trials, TAVI became established as the treatment of choice in elderly patients with AS. Comprehensive geriatric assessment improves health outcomes by allowing steps to be taken to deal with potentially modifiable situations of frailty.4 The aims of this study were: a) to study the clinical, functional, mental, and social characteristics of elderly patients with symptomatic severe AS who are to undergo valve replacement, and b) to analyze the possible presence of undiagnosed diseases, situations of frailty, functional dependence, and cognitive decline.
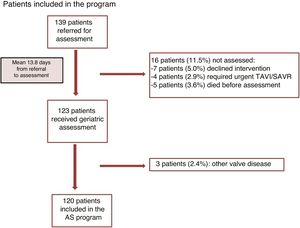
This was a longitudinal, prospective, observational study, which included consecutive patients older than 75 years old with symptomatic severe AS referred for TAVI or surgical aortic valve replacement and assessed by the multidisciplinary Heart Team, between 1 May 2018 and 30 April 2019 (figure 1).
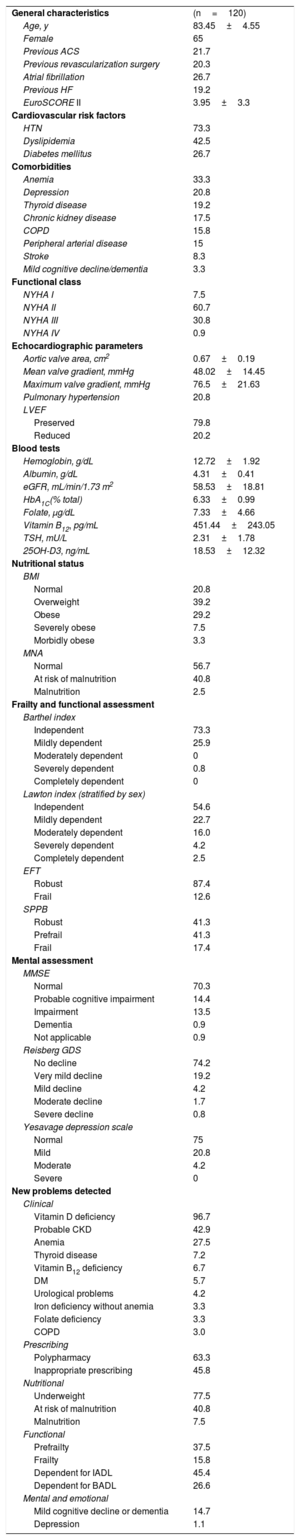
The characteristics of the study population are given in table 1. A total of 79.8% of the patients were aged 80 years or older. The most prevalent comorbidities were hypertension, dyslipidemia, and anemia, with a mean score on the Short-Form Charlson Comorbidity Index of 2.47±2. We found a mean 9.01±3.11 previously-diagnosed medical conditions, 2.01±1.89 previous operations and a mean 6.99±3.4 long-term repeat-prescription medications. Mean body mass index was 29.05±5.53 and mean Mini Nutritional Assessment Short Form score was 11.33±1.69 (within the range for normal/at risk of malnutrition). Functional assessment detected a high level of independence for activities of daily living (mean scores on Barthel index, 93.04±11.64, and on the Lawton scale, 5.79±2.06). On frailty assessment, the mean Essential Frailty Toolset score was 1.28±1.08 (within the robust range) and the mean Short Physical Performance Battery score was 8.67±2.47 (in the prefrail range). On mental assessment, the mean Mini-Mental State Examination score was 26.65±3.39, mean score on Reisberg’ Global Deterioration Scale was 1.38±0.77, and mean score on Yesavage's Geriatric Depression Scale was 3.08±2.68 (corresponding to no cognitive or affective impairment). Regarding social situation, the mean score on the Gijón assessment scale was 6.35±1.87, with 100% of patients obtaining results within the “no social risk” range.
Baseline characteristics of the study population and new problems detected
| General characteristics | (n=120) |
| Age, y | 83.45±4.55 |
| Female | 65 |
| Previous ACS | 21.7 |
| Previous revascularization surgery | 20.3 |
| Atrial fibrillation | 26.7 |
| Previous HF | 19.2 |
| EuroSCORE II | 3.95±3.3 |
| Cardiovascular risk factors | |
| HTN | 73.3 |
| Dyslipidemia | 42.5 |
| Diabetes mellitus | 26.7 |
| Comorbidities | |
| Anemia | 33.3 |
| Depression | 20.8 |
| Thyroid disease | 19.2 |
| Chronic kidney disease | 17.5 |
| COPD | 15.8 |
| Peripheral arterial disease | 15 |
| Stroke | 8.3 |
| Mild cognitive decline/dementia | 3.3 |
| Functional class | |
| NYHA I | 7.5 |
| NYHA II | 60.7 |
| NYHA III | 30.8 |
| NYHA IV | 0.9 |
| Echocardiographic parameters | |
| Aortic valve area, cm2 | 0.67±0.19 |
| Mean valve gradient, mmHg | 48.02±14.45 |
| Maximum valve gradient, mmHg | 76.5±21.63 |
| Pulmonary hypertension | 20.8 |
| LVEF | |
| Preserved | 79.8 |
| Reduced | 20.2 |
| Blood tests | |
| Hemoglobin, g/dL | 12.72±1.92 |
| Albumin, g/dL | 4.31±0.41 |
| eGFR, mL/min/1.73 m2 | 58.53±18.81 |
| HbA1C(% total) | 6.33±0.99 |
| Folate, μg/dL | 7.33±4.66 |
| Vitamin B12, pg/mL | 451.44±243.05 |
| TSH, mU/L | 2.31±1.78 |
| 25OH-D3, ng/mL | 18.53±12.32 |
| Nutritional status | |
| BMI | |
| Normal | 20.8 |
| Overweight | 39.2 |
| Obese | 29.2 |
| Severely obese | 7.5 |
| Morbidly obese | 3.3 |
| MNA | |
| Normal | 56.7 |
| At risk of malnutrition | 40.8 |
| Malnutrition | 2.5 |
| Frailty and functional assessment | |
| Barthel index | |
| Independent | 73.3 |
| Mildly dependent | 25.9 |
| Moderately dependent | 0 |
| Severely dependent | 0.8 |
| Completely dependent | 0 |
| Lawton index (stratified by sex) | |
| Independent | 54.6 |
| Mildly dependent | 22.7 |
| Moderately dependent | 16.0 |
| Severely dependent | 4.2 |
| Completely dependent | 2.5 |
| EFT | |
| Robust | 87.4 |
| Frail | 12.6 |
| SPPB | |
| Robust | 41.3 |
| Prefrail | 41.3 |
| Frail | 17.4 |
| Mental assessment | |
| MMSE | |
| Normal | 70.3 |
| Probable cognitive impairment | 14.4 |
| Impairment | 13.5 |
| Dementia | 0.9 |
| Not applicable | 0.9 |
| Reisberg GDS | |
| No decline | 74.2 |
| Very mild decline | 19.2 |
| Mild decline | 4.2 |
| Moderate decline | 1.7 |
| Severe decline | 0.8 |
| Yesavage depression scale | |
| Normal | 75 |
| Mild | 20.8 |
| Moderate | 4.2 |
| Severe | 0 |
| New problems detected | |
| Clinical | |
| Vitamin D deficiency | 96.7 |
| Probable CKD | 42.9 |
| Anemia | 27.5 |
| Thyroid disease | 7.2 |
| Vitamin B12 deficiency | 6.7 |
| DM | 5.7 |
| Urological problems | 4.2 |
| Iron deficiency without anemia | 3.3 |
| Folate deficiency | 3.3 |
| COPD | 3.0 |
| Prescribing | |
| Polypharmacy | 63.3 |
| Inappropriate prescribing | 45.8 |
| Nutritional | |
| Underweight | 77.5 |
| At risk of malnutrition | 40.8 |
| Malnutrition | 7.5 |
| Functional | |
| Prefrailty | 37.5 |
| Frailty | 15.8 |
| Dependent for IADL | 45.4 |
| Dependent for BADL | 26.6 |
| Mental and emotional | |
| Mild cognitive decline or dementia | 14.7 |
| Depression | 1.1 |
25OH-D3: vitamin D; ACS, acute coronary syndrome; BADL, basic activities of daily living; BMI, body mass index; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; EFT, Essential Frailty Toolset; eGFR, estimated glomerular filtration rate; HbA1C, glycated hemoglobin; HF, heart failure; HTN, hypertension; IADL, instrumental activities of daily living; LVEF, left ventricular ejection fraction; MMSE, Mini-Mental State Examination; MNA, Mini Nutritional Assessment Short Form; NYHA, New York Heart Association; Reisberg GDS, Reisberg's global deterioration scale; SPPB, Short Physical Performance Battery; TSH, thyroid-stimulating hormone.
Values are expressed as n (%) or mean±standard deviation.
Following comprehensive geriatric assessment, there was a mean 6±2.36 new diagnoses per patient (720 in total). Undiagnosed vitamin D deficiency with no known history was identified in 96.7%, and severe deficiency in 17.4%. Polypharmacy was diagnosed in 63.3% of patients; benzodiazepine prescription was the most common inappropriate prescription (37.5%). Suboptimal prescription was identified in 4.2% of patients and treatment nonadherence in 1.7%. Malnutrition or risk of malnutrition was present in 43.3% of the patients and hypoalbuminemia in 5.8%. Rates of frailty varied between 12.6% and 17.4% depending on the screening tool used. Some degree of functional dependence for basic activities of daily living was present in 26.7%, while functional dependence for instrumental activities of daily living was found in 45.4%. Previously undiagnosed mild cognitive decline or dementia was present in 14.7%; depression was found in 1.1% of patients with no previous history, and adjustment disorder or anxiety was identified in 10.8%.
The main finding in our study was that elderly patients with severe AS referred for valve replacement had similar levels of comorbidity, polypharmacy, and malnutrition to those identified in other populations such as in the CGA-TAVI multicenter registry5 or the FRAILTY-AVR Study,6 although the scores from the tools that specifically evaluate frailty indicated that they were slightly more robust. They also had undiagnosed conditions including vitamin deficiencies, chronic kidney disease, anemia, diabetes, thyroid disease, nutritional problems, and mild cognitive decline. We also found situations of frailty and functional dependency amenable to intervention and, likely, reversal. The detection of all these problems through a comprehensive geriatric assessment is essential, as it lays the foundations for a future analysis to determine whether a multicomponent low-intensity physical exercise program prior to valve replacement could help improve these patients’ care process and health outcomes. Our study has 2 main limitations: it was a single-center study and it involved a selected population (patients referred to the multidisciplinary Heart Team). As a strength, our study is the first to routinely perform, in all patients, a comprehensive geriatric assessment including nutritional, functional, mental, and frailty assessment, with a specific focus on detecting undiagnosed problems.