Keywords
INTRODUCTION
Budd-Chiari syndrome is a heterogeneous group of diseases characterized by occlusion of the hepatic veins or the inferior vena cava, producing portal hypertension. The most frequent cause in Western countries is thrombotic occlusion in a hypercoagulable state.1 The present case illustrates percutaneous recanalization of complete inferior cava occlusion by angioplasty and stent implantation in a patient with primary antiphospholipid syndrome.
CASE STUDY
A 47-year old man with primary antiphospholipid syndrome and associated Budd-Chiari syndrome was hospitalized several times for abdominal pain, tension ascites, and refractory edema, despite anticoagulant treatment and high doses of furosemide and spironolactone. Magnetic resonance angiography showed total occlusion of the inferior intrahepatic vena cava, immediately above the junction of the suprahepatic veins, which were patent. We were advised to attempt percutaneous recanalization.
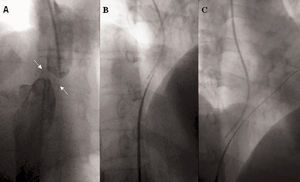
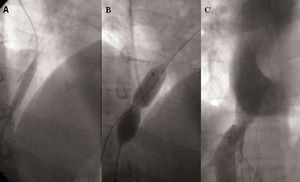
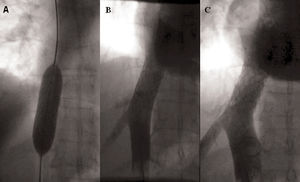
The right femoral and internal jugular veins were canalized and a complete membranous obstruction was observed in the inferior vena cava, at a distance of 20 mm from the junction with the right atrium (Figure 1A). Via the right femoral approach, the membrane was perforated using a Brockenbrough transseptal needle and a Mullins sheath (Cook Europe, Bjaeverskov, Denmark), under fluoroscopic guidance in several views (Figure 1B). A small amount of contrast material was injected during the process of penetrating the membrane to assure proper needle angle. After perforating the occlusion, normal positioning in the junction of the right atrium was confirmed with contrast injection. Using a right femoral approach, a 290-mm PT Graphix intermediate angioplasty guidewire (Boston Scientific Scimed, Plymouth, Minnesota, USA) was inserted through the Brockenbrough needle and the needle was withdrawn (Figure 1C). Subsequently, balloons of increasing caliber were advanced through the Mullins sheath over the guidewire, dilating the obstruction in successive steps. We first used a 3-mm CrossSail balloon (Guidant Corp., Temecula, California, USA) and then a 5-mm Diamondback balloon (InSitu Technologies, Inver Grove Heights, Minnesota, USA) (Figure 2A). Finally, a 16-mm Bonhoeffer Multitrack balloon for mitral valvuloplasty (NuMED, Hopkinton, New York, USA) was inflated (Figure 2B) and the formation of a new lumen became visible (Figure 2C). Nevertheless, there was significant elastic recoil, leaving a residual peak-to-peak gradient of 10 mm Hg. Given the outcome, the decision was made to perform a second procedure with stent implantation. In this second procedure, again via the right femoral vein, predilation with a Maxi LD balloon (20x80 mm) (Cordis, Johnson & Johnson, Miami, Florida, USA) was performed at 4 atm, and a 40-mm length Palmaz stent (P 4014) (Cordis, Johnson & Johnson, Miami, Florida, USA) was inserted over the balloon catheter. The procedure was successful and there was no residual gradient (Figure 3A and B). Right-sided follow-up catheterization at 12 months after stent implantation showed no significant restenosis (Figure 3C). At the follow-up over two years later, the patient remains asymptomatic and has not required diuretic treatment.
Fig. 1. A: angiographic image of membranous occlusion. B: the occlusion is perforated with a Brockenbrough needle. C: angioplasty guidewire in the right atrium through the needle.
Fig. 2. A: dilation with angioplasty balloon. B: the narrowing is visible during dilation with a Multitrack valvuloplasty balloon. C: recanalization of the inferior vena cava after balloon dilation.
Fig. 3. A: process of stent implantation in the vena cava. B: immediate final result of stent placement. C: follow-up angiography at 12 months.
DISCUSSION
The angiographic study in this patient showed complete membranous occlusion of the inferior vena cava. Formerly, this type of occlusion was considered to have a congenital origin. However, based on findings obtained with new imaging techniques and histological studies, it has been postulated that the membranes are the sequelae of a thrombotic process.2 This theory is logical in the patient presented, with a hypercoagulable state and primary antiphospholipid syndrome.
Treatment for Budd-Chiari syndrome varies according to the etiology and level of the obstruction. In cases of complete or segmental occlusion of the inferior vena cava, the use of percutaneous revascularization procedures is increasingly more common, whereas surgery is reserved for cases that cannot be resolved percutaneously.3,4 The procedure can be performed safely under fluoroscopic guidance in several views to assure proper angling of the needle as it perforates the membrane.5 Balloon angioplasty offers good initial results, although the rate of restenosis varies from 3% to 48% according to the series.5,6 As compared to results with the balloon, stenting improves the long-term outcome as it reduces the incidence of restenosis.7
In conclusion, percutaneous revascularization for complete vena cava occlusion in a patient with Budd-Chiari syndrome was a safe procedure that proved long-term effectiveness.
ACKNOWLEDGEMENT
We are grateful to Dr. Fernando Olías de la Cruz for his invaluable help in preparing the photographic images.
Correspondence: Dr. A. Sánchez Recalde.
Unidad Médico-Quirúrgica de Cardiología. Hospital Universitario La Paz.
P.o de la Castellana, 261. 28046 Madrid. España.
E-mail: recalde@secardiologia.es