Keywords
INTRODUCTION
A syndrome characterized by transient akinesia or dyskinesia primarily affecting the left ventricular apex, without coronary artery lesions and triggered by physical or psychological stress has been described in recent years, mainly in Japan. The entity is now known as left ventricular apical ballooning but was previously called "ampulla cardiomyopathy" or "takotsubo cardiomyopathy."1 Few cases have been described in Spain although the similarity between this entity and acute coronary syndrome implies probable underdiagnosis.2,3 The pathophysiology of this syndrome is unknown but data suggest that abnormal autonomous cardiac activity may be involved.1
We describe the case of a woman who developed severe ventricular dysfunction and cardiogenic shock following intense emotional stress, followed by complete recovery of left ventricular systolic function. Sympathetic cardiac activity, studied by 123I-metaiodobenzyl guanidine (MIBG) scintigraphy, markedly decreased, supporting the theory that abnormal autonomous functional sympathetic innervation was the pathophysiologic base of her condition.
CLINICAL CASE
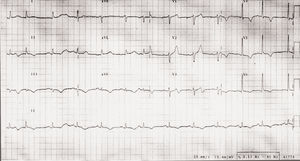
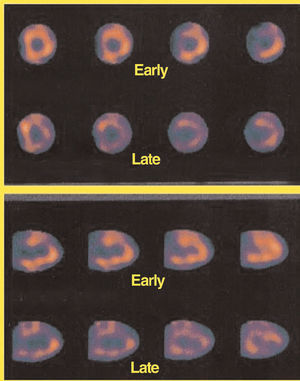
Our patient was a 68-year-old woman with a history of hypertension and hyperthyroidism following the removal of a multinodular goiter. Six years earlier she had received a dual chamber pacemaker implant indicated for diseased sinus node and was currently under treatment with enalapril and thyroid hormones. She presented at the Emergency Room following intense emotional stress (she had witnessed an accident involving her son) with retrosternal pain spreading to neck and shoulders and dyspnea of 2 hours duration. Initial physical examination revealed nothing of note with a blood pressure of 100/60 mm Hg and a heart rate of 70 beats/min. An electrocardiogram (ECG) indicated repolarization abnormalities with T-wave inversion from V3 to V6 and in the inferior leads (Figure 1). The patient also had elevated troponin I (2.5 ng/mL). The patient was also diagnosed with an acute coronary syndrome and admitted to the coronary care unit and treated with acetylsalicylic acid, clopidogrel, enoxaparin, nitrates, and beta-blockers. Initial evolution was unfavorable and the patient developed cardiogenic shock. The maximum troponin level was the first value and serial values of creatine kinase-MB isoenzyme were normal. An echocardiogram (ECHO) showed akinesia of all medial and apical segments with good left ventricular systolic function of basal segments, severely depressed ejection fraction (15%), moderate mitral regurgitation with normal valve and subvalvular apparatus, without intraventricular gradient. Cardiac catheterization at 12 hours after admission revealed an absence of coronary artery lesions. Ventriculography was not performed to avoid further deterioration of an already unstable hemodynamic situation. In the following days, after treatment with dopamine, dobutamine and diuretic, her hemodynamic condition improved progressively. The ECG showed normalization of the repolarization abnormalities and an ECHO performed 1 week after admission showed complete recovery of normal left ventricular systolic function. One after admission, ECHO showed absence of mitral regurgitation. Thyroid hormone data were normal. A diagnostic study for etiologic agents of myocarditis gave negative results. At 4 weeks, the patient underwent planar MIBG cardiac scintigraphy and simple photon emission computed tomography (SPECT) at 15 min and 4 hours after injection of 185 MBq of the isotope, giving a heart to mediastinic ratio of 1.68 in the early phase and 1.38 in the late phase (both below the reference values, especially for the late phase), with reduced uptake in the SPECT (Figure 2). One week later the patient was discharged, asymptomatic, receiving treatment with aspirin, enalapril and pravastatin and she continued this regime at 4-month follow-up.
Fig. 1. Electrocardiogram at admission shows repolarization abnormalities with T-wave inversion of V3 to V6, II, III, and aVF.
Fig. 2. MIBG scintigraphy SPECT images. In the upper part we see images that correspond to the short-axis and in the lower part, the vertical long-axis. The minimal isotope uptake can be seen, especially in the later phases. MIBG indicates 123I-metaiodobenzyl guanidine cardiac scintigraphy; SPECT, simple photon emission computed tomography.
DISCUSSION
Presence of transient ventricular dysfunction has been described in a range of clinical situations such as post-ischemic myocardial stunning,4 myocarditis,5 subarachnoid hemorrhage,6 pheochromocytoma crisis,7 and transient left ventricular apical ballooning (TLVAB), primarily described in Japan and better known following publication of the Tsuchihashi et al1 series of 88 patients. This syndrome is characterized by appearing principally in women, following physical or emotional stress, and involving chest pain, ECG abnormalities, transient akinesia at the apex of the left ventricle and normal coronary arteries. The illness is generally benign with intrahospital mortality of 1% although complications such as arrhythmias, heart failure, dynamic subaortic stenosis, cardiogenic shock, and embolic stroke have been described.1-3
The case we describe demonstrates the principal characteristics of TVLAB with peculiarities such as initial ECG abnormalities consisting of T-wave inversion. This is practically universal in the syndrome (97%) but usually follows ST segment elevation which we did not find in this patient, perhaps due to the time course.
The patients' left ventricular systolic function was extensively altered but evidenced typical characteristics in the basal segments and the ECHO showed the typical left ventricular cavity morphology that initially gave its name to this entity: "ampulla cardiomyopathy" or "takotsubo cardiomyopathy." The patient also had moderate mitral regurgitation that was probably related to papillary muscle dysfunction since we found no morphological alteration of the valve and regurgitation disappeared on recovery of normal left ventricular systolic function. To our knowledge, transient mitral regurgitation has only been described in 1 previous case.3
Initially, our patient presented an unstable hemodynamic situation prior to cardiogenic shock, but responded favorably to treatment. Tsuchihashi et al1 reported cardiogenic shock in 15% of patients with a similarly benign evolution,1 as it did not cause the death of any of the patients. This distinguishes it from the known poor prognosis for cardiogenic shock from other causes such as ischemia.
Although the pathophysiology of TLVAB syndrome is unknown, some data suggest a transient abnormality in sympathetic cardiac activity induced by physical or mental stress. This abnormality has been demonstrated in MIBG cardiac scintigraphy.8 MIBG is an analogous of noradrenalin with radioactive iodine, which is captured and stored in sympathetic nerve endings; uptake uses the same mechanism as noradrenalin transport making it an indicator of sympathetic nerve activity. Both autonomic dysfunction in patients with diabetes9 and reinnervation following heart transplantation10 have been studied with MIBG cardiac scintigraphy. In our case, MIBG scintigraphy performed one month after admission showed considerably reduced isotope uptake suggesting noradrenalin depletion in sympathetic cardiac nerve endings, which would concur with earlier studies.8 Stress triggers sudden, intense release of cardiac noradrenalin that, as in pheochromocytoma crisis or subarachnoid hemorrhage, would cause myocardial dysfunction8 either directly or by inducing an intraventricular gradient.3 Scintigraphic results would be the consequence of noradrenalin loss in the sympathetic terminal. It is well known that noradrenalin can cause direct myocardial damage and, although vasospasm has been considered a possibility, several studies have found this to be rare.1,11 With this pathophysiologic hypothesis in mind, we should consider the possible benefit of early administration of beta-blockers in these patients.
In conclusion, the case we describe a case of TLVAB syndrome with the unusual presence of cardiogenic shock with a favorable prognosis and the discovery of transient mitral regurgitation. The anomalies revealed by MIBG cardiac scintigraphy indicate sympathetic nervous system abnormalities as a pathophysiologic base.
Correspondence: Dr. J.C. Gallego Page.
Servicio de Cardiología. Complejo Hospitalario Universitario de Albacete. Hermanos Falcó, s/n. 02006 Albacete. España.
E-mail: jgallegop@secardiologia.es