In recent decades, the use of arterial grafts in coronary revascularization surgery has increased due to the good long-term outcomes achieved. Internal mammary artery grafting has the best long-term patency rate, the best survival rate, and the least need for intervention compared with other grafts.1 Since the introduction of radial artery (RA) grafting, this technique has been used preferentially over other arterial grafts because of its low in-hospital mortality, reduced rate of perioperative myocardial infarction, and acceptable patency rate (92% at 1 year and 88% at 10 years).2,3 This superior patency rate compared with other arterial and venous grafts4 is due to the biological properties of the RA, such as adaptation to blood flow, reduced proliferation of arterial intima, and reduced tendency to develop atherosclerosis.5
In recent decades, noninvasive imaging techniques have allowed direct visualization of atherosclerotic disease of the coronary arteries and arterial and venous grafts and have shown an excellent correlation with invasive angiography.6
The aims of this study were to assess the patency of arterial grafts (mainly RA) using cardiac computed tomography (CT) and to compare patency on CT with that observed on invasive angiography. In addition, we analyzed the relationship between RA graft dysfunction and clinical, anatomical, and surgical variables, as well as the short- to medium-term prognostic impact of such dysfunction.
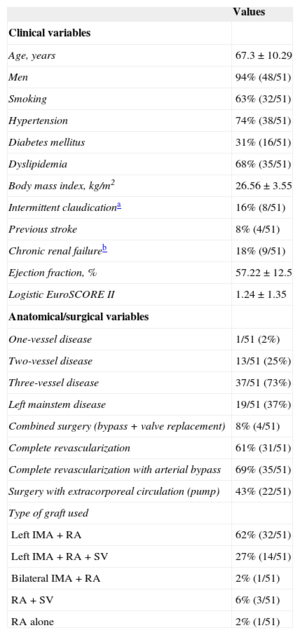
This study prospectively included 51 unselected consecutive patients who underwent coronary artery revascularization (with at least one RA graft) in our hospital from 2010 to 2012. The preoperative clinical, anatomical, and surgical data are shown in the Table. All patients had postoperative cardiac CT (mean time between surgery and CT was 203 days ± 46 days), and clinical follow-up (median 847 days, interquartile range 357 days) to evaluate the incidence of adverse clinical events (death, myocardial infarction with or without ST-elevation, need for revascularization, heart failure, or angina with documented myocardial ischemia).
Table Clinical, Anatomical, and Surgical Patient Variables
| Values | |
|---|---|
| Clinical variables | |
| Age, years | 67.3 ± 10.29 |
| Men | 94% (48/51) |
| Smoking | 63% (32/51) |
| Hypertension | 74% (38/51) |
| Diabetes mellitus | 31% (16/51) |
| Dyslipidemia | 68% (35/51) |
| Body mass index, kg/m2 | 26.56 ± 3.55 |
| Intermittent claudicationa | 16% (8/51) |
| Previous stroke | 8% (4/51) |
| Chronic renal failureb | 18% (9/51) |
| Ejection fraction, % | 57.22 ± 12.5 |
| Logistic EuroSCORE II | 1.24 ± 1.35 |
| Anatomical/surgical variables | |
| One-vessel disease | 1/51 (2%) |
| Two-vessel disease | 13/51 (25%) |
| Three-vessel disease | 37/51 (73%) |
| Left mainstem disease | 19/51 (37%) |
| Combined surgery (bypass + valve replacement) | 8% (4/51) |
| Complete revascularization | 61% (31/51) |
| Complete revascularization with arterial bypass | 69% (35/51) |
| Surgery with extracorporeal circulation (pump) | 43% (22/51) |
| Type of graft used | |
| Left IMA + RA | 62% (32/51) |
| Left IMA + RA + SV | 27% (14/51) |
| Bilateral IMA + RA | 2% (1/51) |
| RA + SV | 6% (3/51) |
| RA alone | 2% (1/51) |
IMA, internal mammary artery; RA, radial artery; SV, saphenous vein
The CT was performed with a 256-slice scanner (iCT 256, Philips Healthcare, Amsterdam, Netherlands) and the images were analyzed in off-line work stations (median effective irradiation of 7.5 mSv, interquartile range 3.76 mSv). Severe coronary stenosis was defined as a reduction of at least 70% in luminal diameter (compared with the reference luminal diameter), and RA grafts were considered occluded in the absence of flow or the presence of “string sign”. Significant luminal graft stenoses were subsequently assessed using invasive angiography.
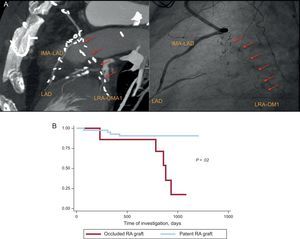
A total of 130 arterial grafts were studied on cardiac CT (77 from the radial artery, 52 from the internal mammary artery, and 1 from the right mammary artery), with a mean of 3 bypasses per patient (150 bypasses, 51 patients). No patients had documented ischemic or functional complications in the ipsilateral upper limb of the excised RA graft. The patency rate of the grafts, evaluated with CT, was 100% (52 of 52) for internal mammary artery and right mammary artery, and 91% (70 of 77) for RA. All RA grafts considered occluded on CT were confirmed with invasive angiography (7 of 7, kappa index +1, P < .05) (Figure A).
A: Occlusion left radial artery bypass to obtuse marginal artery. Anatomical correlation between invasive angiography and 256-slice cardiac tomography. B: Kaplan-Meier event-free survival curves. IMA-LAD, internal mammary artery to left anterior descending artery; LAD, left anterior descending artery; LRA-OMA, left radial artery to obtuse marginal artery; RA, radial artery.
On univariate analysis, the clinical, analytical, and anatomical variables showing a statistically significant association with RA graft occlusion were diabetes mellitus (P = .01), low preoperative hemoglobin level (P = .02), native coronary artery disease (prior to RA bypass anastomosis) with < 90% stenosis (P = .01), and the use of noradrenaline in the immediate postoperative period (P < .001). The variables not showing a statistically significant association with RA graft occlusion at follow-up were logistic EuroSCORE II preoperative risk, type of revascularization surgery (with or without extracorporeal circulation), peak high-sensitivity troponin T, and duration of postoperative stay (P > .05 for all variables).
At postoperative clinical follow-up, 11% of patients with a patent RA graft (4 of 44) and 71% of patients with an occluded RA graft (5 of 7) had an adverse event (Figures A and B). In patients with an occluded RA graft, adverse events consisted of 2 episodes of decompensated heart failure and 3 non--ST-elevation acute coronary syndromes. Of the 5 patients admitted for adverse events, 3 underwent revascularization using percutaneous angioplasty with stenting, the native vessel not being protected due to RA graft occlusion.
This study confirms the excellent diagnostic precision of cardiac CT compared with invasive angiography in the assessment of RA grafts. We found that the short- to medium-term patency of RA grafts was reduced in patients with diabetes, in those with < 90% stenosis of the native coronary bed, and in those who required vasoactive support in the immediate postoperative period. This tudy also showed that RA leads to a substantial increase in adverse events in the short- to medium-term, suggesting the need for systematic patency screening, as is done in the postoperative study of patients after surgical valve replacement.