Acute myocarditis is an inflammatory process affecting the myocardium that mainly occurs secondary to a viral infection. The definitive diagnosis is established by endomyocardial biopsy,1 but because this method is invasive, it is performed only in selected patients. A presumptive diagnosis can be reached by taking a clinical history and performing noninvasive complementary tests.1,2 Among these, cardiac magnetic resonance (CMR) imaging plays an important role, and experience with this technique is increasing in children.3 CMR can detect the tissue changes inherent to myocarditis, such as edema, hyperemia, and necrosis. To establish the diagnosis, at least 2 of the 3 CMR criteria must be fulfilled.4 The sensitivity of the test varies according to the clinical pattern: sensitivity is very high in the forms presenting with precordial pain, but is lower in patients with dilatation and ventricular dysfunction. In these patients, the differential diagnosis should be made with other conditions such as dilated cardiomyopathy or noncompaction cardiomyopathy. This latter disease can present with a pattern of heart failure at any age, and the diagnosis is established on the basis of echocardiographic5 and CMR6 criteria.
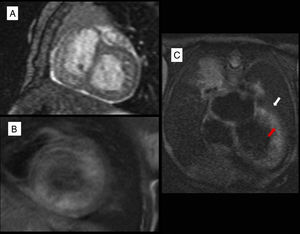
We present a series of 3 patients admitted to our center between April 2015 and September 2016 with clinical signs and symptoms of cardiogenic shock. The patients’ characteristics are described in Table. All required inotropic support and mechanical ventilation. After they had been stabilized, the patients were extubated, and standard heart failure therapy was initiated. The first 2 patients had experienced an infectious process before symptom onset. At admittance they underwent electrocardiography, echocardiography, blood analysis to determine myocardial injury markers, and polymerase chain reaction (PCR) testing for cardiotropic viruses in blood and respiratory secretions. CMR was performed during the first 3 days following admittance, with the patients under sedation and breathing spontaneously. Only 1 patient tested PCR-positive in a blood sample, with detection of parvovirus B19 (Table). All 3 patients had left ventricular dilatation and hypertrabeculation, and they met the diagnostic criteria of noncompaction cardiomyopathy both on CMR and echocardiography.5,6 There was a good correlation between the ejection fraction determined by CMR and the estimated value obtained with the Teichholz formula on echocardiography (Table). A hyperintense signal on CMR T2 sequences and increased early gadolinium uptake were seen in all patients. Of note, both the hyperintensity and signal increase in the early phase following gadolinium administration were localized at the trabeculated region, but did not reach the compacted myocardium (Figure). In the second and third patient, the right ventricle also showed considerable trabeculation. In the first patient, who tested PCR-positive for parvovirus B19 in blood and had a poor clinical course, endomyocardial biopsy was carried out. The results were normal, and diagnosis of acute myocarditis was ruled out. Thus, the diagnostic orientation in the 3 patients was noncompaction cardiomyopathy with severe ventricular dysfunction.
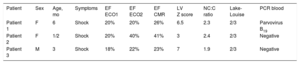
Patient Characteristics
| Patient | Sex | Age, mo | Symptoms | EF ECO1 | EF ECO2 | EF CMR | LV Z score | NC:C ratio | Lake-Louise | PCR blood |
|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | F | 6 | Shock | 20% | 20% | 26% | 6.5 | 2.3 | 2/3 | Parvovirus B19 |
| Patient 2 | F | 1/2 | Shock | 20% | 40% | 41% | 3 | 2.4 | 2/3 | Negative |
| Patient 3 | M | 3 | Shock | 18% | 22% | 23% | 7 | 1.9 | 2/3 | Negative |
EF CMR, ejection fraction on cardiac magnetic resonance imaging; EF ECO1, ejection fraction on echocardiography at the time of the diagnosis; EF ECO2, ejection fraction on echocardiography at the time cardiac magnetic resonance was performed; F, female; Lake-Louise, number of myocarditis diagnostic criteria fulfilled on cardiac magnetic resonance; NC:C, ratio of the non-compacted to compacted segment in diastole, measured by cardiac magnetic resonance; PCR, polymerase chain reaction; M, male; LV Z score, left ventricular Z score on echocardiography.
A: SSFP (steady-state free precession) short-axis cine sequence showing lateral wall trabeculation. B: T1 sequence in the early phase following gadolinium administration; the left ventricular internal wall (trabeculated region) is hyperintense relative to the external wall (compacted myocardium). C: T1 sequence, 4-chamber view shows a hyperintense area in the trabeculated region (red arrow) relative to the compacted region (white arrow).
At the time of writing, the 3 patients have been stable, show moderate-severe ventricular dysfunction, and are receiving heart failure treatment.
In conclusion, we wish to convey the usefulness of CMR for the etiological diagnosis of ventricular dysfunction in pediatric patients. This technique should be among the first to be used in these patients, as it can avoid the need for invasive examinations that are not without risk, such as endomyocardial biopsy. This procedure should be carried out in selected patients, particularly in the pediatric population. In infants with noncompaction cardiomyopathy and severe left ventricular dysfunction, the differential diagnosis with acute myocarditis can be challenging. Trabeculation appears hyperintense on T2 images and slow flow due to severe ventricular dysfunction may lead to gadolinium retention in the intertrabecular spaces. The absence of the characteristic myocarditis pattern of edema and patchy subepicardial hyperemia, and the lack of late contrast uptake can guide the diagnosis toward ventricular dysfunction secondary to noncompaction cardiomyopathy.
.