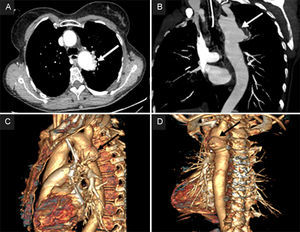
A 57-year-old woman was admitted to the emergency room of our hospital for sudden lipothymia and copious hemoptysis. Twenty-seven years previously she had undergone Dacron patch aortoplasty for aortic coarctation with the Cooley technique.1 On admission, the patient was hypotensive, dyspneic and anemic (Hb 6.3mg/dL). A computed tomography scan showed a 36-mm pseudoaneurysm in the proximity of the aortic isthmus, perforated through a 6-mm fistula into the posterolateral aspect of the left lung (Figure 1A-D).
Computed tomography angiography scan shows the 36-mm pseudoaneurysm (arrows), located 13mm distal to the origin of the left subclavian artery, perforated through a 6-mm fistula with the bronchial tree. A: 2D computed tomography angiography scan, axial view. B: 2D coronal view. C: 3D sagittal plane reconstruction. D: 3D left posterior reconstruction. Arrows show the 36 mm pseudoaneurysm located 13 mm distal to the origin of the left subclavian artery, perforated through a 6 mm fistula with the bronchial tree.
Thoracic endovascular aortic repair was not indicated due to unsuitable vascular access and lack of appropriate landing zones for endograft placement. The patient underwent emergency surgical reoperation.
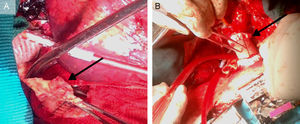
The chest was entered through a fourth intercostal space left thoracotomy. The proximal thoracic aorta immediately distal to the left subclavian artery and the descending aorta at the seventh intercostal space level were isolated for subsequent cross clamping. At the level of the previously coarctated segment, a pseudoaneurysmatic dilatation of the aorta was observed, tenaciously adherent to the left upper pulmonary lobe. On moderate (32°C) hypothermic cardiopulmonary bypass, by using left femoral vein drainage and dual femoral artery and distal aortic arch arterial return, the descending aorta was proximally and distally cross clamped. The pseudoaneurysm was partially dissected free and was then excised, leaving the anteromedial wall attached to the lung, thus penetrating into the pulmonic parenchyma. The Dacron patch showed a 1-cm disruption of the suture line (Figure 2A).
A: operative findings: the Dacron patch, a segment of the aortic wall at the level of the suture line dehiscence and periaortic inflammatory tissue (arrow) are evident. B: the surgical repair: Dacron tube graft descending aorta reconstruction (arrow), with suture line being reinforced by Teflon strips. The site of the aortic arch cannulation is also quite evident.
The continuity of the descending thoracic aorta was reconstructed with a 24-mm Dacron tube graft (Figure 2B). The patient was hemodynamically stable after the intervention, with no evidence of hemorrhage, but unfortunately died 2 months later from sepsis.
Aortic coarctation represents approximately 5% of all congenital heart malformations, with an incidence of 0.2-0.6 per 1000 live births.2 Surgical correction in young patients is indicated and many techniques have been proposed. The longitudinal Dacron patch aortoplasty of the aortic constricted segment is preferred by many surgeons as it potentially allows subsequent growth of the aortic wall and reduces the number of collaterals to be tied off. Several postoperative complications have been described, such as restenosis, aneurysm, and pseudoaneurysm, frequently developing many years after the intervention.3
Aneurysm and pseudoaneurysm may occur in up to 10% of patients, at a mean interval from operation superior to 12 years.4
In our patient, disruption of the aortic Dacron patch suture line was evident and clearly generated the pseudoaneurysm, composed of thrombotic material surrounded by fibrous and inflammatory tissue. The progressively expanding pseudoaneurysm, mainly in older patients, may compress and erode the pulmonary parenchyma, leading—as in our patient—to the aortopulmonary fistula.
As previously observed,5 the present case confirms that sudden lipothymia, hemoptysis, and anemia could be clinical signs indicative of aortopulmonary fistula in patients who have undergone aortic coarctation repair even many decades earlier. Lifelong follow-up after coarctation aortoplasy is recommended.