Keywords
INTRODUCTION
Persistent left superior vein cava (LSVC) is the most frequent abnormality of the systemic venous system (0.1%-0.5% of the general population) and is not usually associated with any other cardiac defect. Incidence in congenital heart disease varies (2%-5%) and it is more frequent in stenosis or pulmonary atresia, D-transposition, complete atrioventricular septal defects (CASD), and anomalous pulmonary vein drainage.1-3
The right superior vein cava (RSVC) is absent in 1% of patients with persistent LSVC and frequently associated with alterations of cardiac situs.3
Persistent LSVC usually drains into the right atrium thru the coronary sinus (CS) but in 8% of patients it drains directly into the left atrium (LA) as a consequence of a defect in the wall that separates them (unroofed CS). When this occurs incidence of persistent LSVC is 75%. This combination is usually associated with right atrial isomerism and complete or partial atrioventricular septal defect, especially when substantial interatrial communication (IAC) is present.2,3
We report the case of a 1-month-old infant with situs solitus and CASD, absent RSVC and persistent LSVC draining into the left atrium thru an unroofed CS.
CLINICAL CASE
A 1-month-old boy was referred from another hospital diagnosed with CASD with pulmonary hypertension. Pregnancy and birth had been normal.
The boy presented dyspnea with feeding and minimal weight gain. He was being treated with digitalis and furosemide.
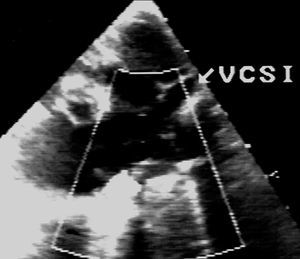
On admission, the boy weighed 3300 g, appeared undernourished, with normal phenotype, tachypnea, 2/4 pansystolic murmur, loud second sound, without hepatomegaly. Chest x-rays revealed cardiomegaly and plethora. The electrocardiogram (ECG) was in sinus rhythm, with a superior QRS axis and biventricular growth. Echocardiography confirmed CASD in situs solitus, a large ostium primum-type CIA, interventricular communication (IVC) partially hidden by common atrioventricular valve chords, cleft mitral valve, right ventricular dominance with viable left ventricle, and LSVC draining into the CS (Figure 1).
Figure 1. Echocardiographic image of persistent left superior vena cava (LSVC).
We performed complete corrective surgery. We found absent RSVC, using the LSVC for cannulation. We used the Carpentier (double patch) technique and acceptable mitral valve competence was achieved. When disconnected from the pump the patient was in nodal rhythm with the sternum open. A few hours later, significant desaturation and mantle or shoulder girdle edema occurred. Echocardiography revealed absence of residual shunt, balanced ventricles and mild tricuspid and mitral valve regurgitation. We did not see the RSVC. Rapid injection of stirred saline solution in an epicranial vein produced microbubbles in the left cardiac cavities. The patient was reoperated immediately without extracorporeal circulation to introduce an 8 mm polytetrafluoroethylene (PTF) conduit between the innominate vein and right atrial appendage and drainage of the LSVC in the left atrium was prevented thru a clip. The patient came out of the operation with normal saturation. The postoperatory period was positive and the patient was discharged at 13 days with a regimen of captopril, furosemide and oral anticoagulants.
DISCUSSION
Few systems are as susceptible to developmental variations and anomalies as those of the principal systemic veins. Although of scarce functional importance, they sometime cause problems in the face of invasive medical-surgical procedures.
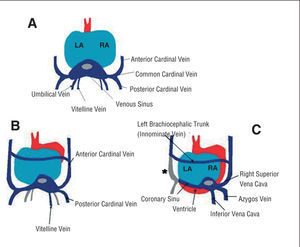
In a 4 mm (week 4) embryo, the principal vein formation that can be distinguished is the sinus vein, where 3 vein groups drain (Figure 2):
Figure 2. Posterior view of the heart of an embryo at 4 weeks (A), 8 weeks (B), and 10 weeks (C) gestation. We see the atrophying of the umbilical veins and of the left vitelline vein (B). The asterisk (C) represents the atrophying of the anterior left cardinal vein (persistent LSVC).
- Vitelline vein system. Transports blood from the vitelline sac.
- Umbilical vein system. Brings blood from the placenta.
- Cardinal vein system, which is completely intraembrionary. The anterior and posterior cardinal veins drain to the right and left of the venous sinus. The common cardinal veins begin at the point where they join.
At 15-17 mm, the right umbilical vein disappears and the left umbilical vein connects distal to the hepatic plexus (venous conduit). The left vitelline vein atrophies and the right vitelline vein contribute to form the inferior vena cava. An anastomosis appears (innominate vein) between the anterior cardinal veins. The common right cardinal will ultimately become the RSVC and the common left cardinal atrophies leaving only a small channel (CS). If this does not atrophy, we call this persistent LSVC draining in the CS.4
Anomalies of superior vena cavae are rare in situs solitus: only occasionally does LSVC draining in the CS appear and it has no hemodynamic consequence. Exceptionally, cyanosis appears in patients with unroofed CS and heterotaxia is then frequent.2,3
Absent RSVC in situs solitus is exceptional (0.1% of patients with cardiomyopathy) and 130 cases had been described prior to 1997. It is associated with LSVC draining in the CS. The RSVC becomes little more than a fibrous chord2,5 and in half of these patients some type of cardiac abnormality is found. More frequent abnormalities are those that affect the CS--above all partial or total unroofed CS--which always drains a LSVC causing cyanosis. These cases are associated with CASD, especially in patients with large CIA.6
Diagnosis of these anomalies is by clinical symptoms and echocardiography. In our patient, the severe desaturation in the postoperatory period was fundamental. In echocardiography, a dilated CS always leads to suspicion of the presence of a LSVC draining in the CS but the diagnosis of defects in the roof makes dilation of the CS less likely.7 Saline contrast echocardiography provided confirmation of LSVC draining in the left atrium.
Echocardiography of RSVC is not systematic but its absence should have been discounted in this patient (CASD with large CIA). Diagnosis prior to surgery or other invasive procedures is important to avoid difficulties in implantation of pacemakers and catheters, cannulation for surgery, cavopulmonary derivation or trasplantation.8,9 Transesophageal echography and magnetic resonance imaging can be of great help in the diagnostic process.10
We should point out the excellent results when correcting complete atrioventricular septal defect with right dominance. In the reoperation, intraatrial correction11 was not contemplated for 2 reasons: a small left atrium in a 1-month-old infant with unbalanced CASD, and to avoid extracorporeal circulation. Nor was direct reconnection of the LSVC with the right atrial appendage viable12 due to the distance between the structures and the aortic interposition. We also rejected using the bidirectional Glenn procedure13 due to pulmonary pressure in CASD. Implantation of a Gore-Tex conduit between the innominate vein and the right atrium has been described in an older child.14 In our patient, we foresee the need for replacement of the conduit for another of a larger caliber.
CONCLUSIONS
Knowledge of absent RSVC is of great interest for correct medical-surgical treatment of children with cardiomyopathy. In patients with CASD, absent RSVC and persistent LSVC oblige us to discount CS roof defects that can complicate the immediate postoperatory period.
Correspondence: Dr. L. Fernández Pineda.
Servicio de Cardiología Pediátrica. Hospital Ramón y Cajal.
Ctra. de Colmenar, km 9,100. 28034 Madrid. España.
E-mail: lfernandezp@hotmail.com