Transcatheter aortic valve implantation increases survival in patients with severe symptomatic aortic stenosis who are not suitable candidates for valve replacement surgery.1 It is not always feasible to employ the usual access routes, transfemoral or transapical, or others such as subclavian artery,2–4 which is increasingly widely used. Implantations via the ascending aorta with anterior minithoracotomy and via the left axillary artery with surgical access or closure have also been described.5
We report the case of a patient with severe symptomatic aortic stenosis, and repeated episodes of heart failure, who underwent aortic valve implantation with a totally percutaneous left axillary approach.
Conventional surgery had been ruled out in this patient due to the high risk associated with his age (85 years) and the presence of combined pulmonary fibrosis and emphysema with highly impaired carbon monoxide diffusing capacity (33.1%), severe chronic renal failure (creatinine clearance, 24mL/min), moderate ventricular dysfunction (left ventricular ejection fraction, 0.40), peripheral arterial disease (presence of aneurysms and stenosis in the iliofemoral artery), and prior coronary revascularization (5 grafts: left internal mammary artery to the left anterior descending artery and right internal mammary artery to ramus intermedius, as well as radial artery T graft to the marginal artery and posterior descending artery). Femoral access was ruled out for endovascular transcatheter aortic valve implantation, because of aortoiliac disease. Subclavian access3 was unacceptable because of the potential risk of impairment to the left and right mammary artery grafts, which were patent. Surgical accesses using minithoracotomy or sternotomy, although not contraindicated, did not appear to be good options due to the severe lung disease and previous surgery. All these clinical conditions prompted the search for alternatives that would involve minimal trauma, in terms of both vascular and respiratory function. Doppler ultrasound revealed that the left axillary artery had an adequate caliber and thickened wall, but there were no atherosclerotic plaques and, therefore, was our access of choice.
The procedure was carried out with the support of the cardiac surgery service, with general anesthesia, orotracheal intubation, and respiratory assistance. Based on transesophageal echocardiography, the aortic annulus diameter was 20mm. A 5-Fr pigtail catheter was advanced from the right femoral artery toward the left axillary artery. From the axillary space, using the point of maximum pulse, with the distal portion of the catheter as the target, and aided by repeated contrast injection to avoid the bifurcation of the subscapular artery, the left axillary artery was cannulated, and a single Prostar XL® closure device (Abbott Vascular) was placed for preclosure (Fig. 1). From the femoral artery, a teflon-coated guide wire was advanced into the left brachial artery to ensure the arterial line in case the subsequent percutaneous closure failed. After placement of an introducer sheath (Cook, 18 Fr), aortic valvuloplasty was performed using a 22-mm balloon (NuCLEUS®, NuMED), and a 26-mm CoreValve® aortic valve (Medtronic, Inc.; Minneapolis, Minnesota, United States) was implanted according to the standard technique (Fig. 2A).
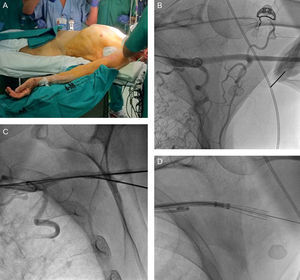
A: Position of the patient for the transaxillary approach, with the arm abducted more than 60°. B: Fluoroscopic image of the angiography of the left axillary artery and external radiopaque marker in an attempt to cannulate the artery. C: Fluoroscopic image at the time of artery cannulation. D: Fluoroscopic image with the Prostar XL® at the moment of ensuring that the 4 needles had backed down into the sheath.
A: Result of the implantation of the CoreValve®. B and D: Residual stenosis after closure of the axillary artery with a single Prostar XL®. C: Degree of stenosis determined by quantitative angiography, which also demonstrates the size of the axillary artery, adequate for the procedure. D, distal; P, proximal.
Hemostasis was achieved immediately and with no problems using the Prostar XL®. Subsequent axillary angiography demonstrated the absence of extravasation and the presence of moderate stenosis that did not jeopardize blood flow (Figs. 2B-D). There were no complications, with the exception of complete atrioventricular block, which required implantation of a dual-chamber pacemaker 24h later. In addition, the patient complained of mild paresthesias, limited to his left hand, with no associated motor deficit, which had disappeared completely 3 months after the procedure.
This is the first report of a case of totally percutaneous axillary access for successful implantation of an aortic prosthesis. We wish to highlight the difficulty of correctly cannulating the left axillary artery from the axillary space, which required fluoroscopic guidance, angiography, and external palpation. The absence of a posterior bone platform and the depth of the artery with respect to the skin contribute to the difficulty of the puncture. In contrast to our procedure, the Hamburg-St. George approach4 is employed in the anterior thoracic wall at the level of the deltopectoral groove, and access to the distal subclavian artery is achieved close to the junction with the axillary artery, and thus, it does not involve the difficulty of a lateral approach.
We wish to stress that detailed study and knowledge of the axillary anatomy and caliber is essential for planning the procedure and deciding on the percutaneous hemostatic closure technique. In our case, we performed quantitative angiography and ultrasound. Although we considered using 2 Proglide® devices (Abbott Vascular), with a smaller diameter than the proximal barrel of the Prostar XL®, which could have minimized injury to the surrounding nerve bundle, we decided to utilize a single Prostar XL® device, based on the axillary artery caliber and on our experience in its use in these procedures. In this respect, the patient only developed self-limiting paresthesias. There were no problems in achieving hemostasis, but vascular complications, such as dissection or perforation, which demand immediate action, can develop. To prevent this, we ensured the arterial line using a Teflon-coated guide wire advanced up to the brachial artery, and had on hand balloons and endoprostheses adjusted to the sizes of the axillary and subclavian arteries, and the support of expert surgeons if all the above failed.
This initial experience of a totally percutaneous intervention broadens once more the possible strategies for transcatheter aortic valve implantation.
.