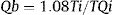
Absolute volumetric coronary blood flow can now be measured invasively by thermodilution due to a new purposely designed monorail microcatheter that allows homogeneous and continuous mixing of room-temperature saline solution with intracoronary blood.1 This microcatheter (Rayflow; Hexacath) has 4 openings at its distal end, and the terminal distal opening is occluded by the guidewire, permitting homogeneous infusion.1 The intracoronary guidewire has a temperature sensor linked to dedicated software (RadiView; Abbott), allowing thermodilution-based measurements of the maximal volume of intracoronary blood per unit of time, according to the formula:
where Ti is the temperature of the infused saline exiting the infusion catheter, T is the temperature of the blood-saline mixture in the distal portion of the coronary artery, and Qi is the preset saline infusion rate through the microcatheter (Figure).1 This procedure can yield quantitative estimates not only of the maximal coronary blood flow (MCF), but also of the corresponding minimal microvascular resistance in the irrigated territory, since this is the ratio of coronary pressure to coronary blood flow, both of which are known.
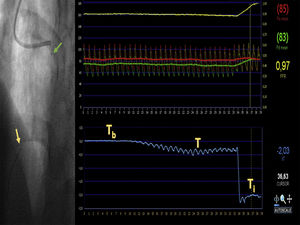
Example measurement of absolute volumetric coronary blood flow. An intracoronary guidewire with a dual pressure and temperature sensor is passed through a guide catheter into the distal segment of the anterior descending coronary artery (yellow arrow). The Rayflow microcatheter is threaded over this guide catheter and advanced into the proximal segment of the artery (green arrow). After connecting the proximal microcatheter tip to an infusion pump, a room-temperature saline solution is infused into the coronary artery at a preset flow rate. The screen displays a real-time readout of the baseline temperature (Tb) and the infusion-induced gradual decrease to a new stable temperature (T). Once the intracoronary temperature stabilizes, the guidewire is withdrawn until the temperature sensor is positioned at the microcatheter tip in order to measure the infusion temperature (Ti). This allows quantitative measurement of maximal volumetric coronary blood flow in the artery according to the formula Qb = 1.08 Ti/T Qi, where Qi is the preset saline infusion rate. Aortic pressure (red trace) and distal coronary pressure (green trace) are monitored simultaneously with the temperature recording; this allows quantitative estimation of fractional flow reserve (yellow trace) and minimal microvascular resistance in the irrigated territory using the formula R = Pd/Qb, where Pd is the distal intracoronary pressure and Qb is the absolute coronary blood flow.
We prospectively recruited 14 patients in whom quantitative coronary angiography revealed no significant coronary lesions (stenosis < 30% of the luminal diameter). In most study participants (11 patients), the indication for coronary angiography was stable angina and a positive or inconclusive exercise treadmill test (6 and 5 patients, respectively). The other 3 patients had ventricular dysfunction with a suspected ischemic etiology. After obtaining informed consent, we carried out an intracoronary evaluation of anterior descending artery function in all patients. A guidewire with a dual temperature and pressure sensor (Certus, Abbot Vascular) was passed through a 6-Fr guide catheter. Physiological parameters were obtained at baseline and after induction of maximal hyperemic flow by perfusion of adenosine (140 μg/kg/min) through the peripheral antecubital vein. The microcatheter was then advanced over the pressure/temperature sensor-tipped guidewire to position its distal extreme in a proximal segment of the artery. Using an infusion pump, saline solution at room temperature was infused through the microcatheter at a rate of 18 mL/min. Once a stable drop in temperature was obtained, the guidewire with the temperature sensor was withdrawn to the microcatheter tip in order to measure the infusion temperature (Figure). All data collection was automated, and data were stored and subsequently analyzed with the specific RadiView software (Abbott).
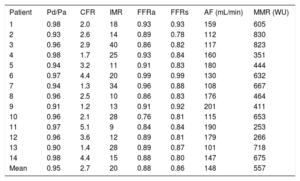
The mean age of the 14 patients was 66 ± 8 years, and 5 (36%) were women. Of the patients, 3 (21%) had diabetes, 10 (71%) hypertension, and 5 (36%) dyslipidemia; 2 (14%) were smokers. The mean interval from guide catheter introduction to completing all measurements was 8.6 ± 6min. The mean time from starting infusion to achieving a stable temperature decrease was 7.6 s. The median MCF was 153mL/min [interquartile range, 114-179mL/min], with a median microvascular resistance of 619 Wood units [396-689 WU] (Table). Median fractional flow reserve showed a tendency to lower values after saline infusion than after adenosine infusion (0.84 vs 0.89; P = .09). In 2 patients (14%), saline and adenosine infusion yielded discrepant assessments of lesion functional significance (with the cutoff set at ≤ 0.80). Among the participants, 1 patient developed a transitory acute arterial occlusion that resolved spontaneously with no complications.2
Intracoronary Hemodynamic Parameters Obtained
| Patient | Pd/Pa | CFR | IMR | FFRa | FFRs | AF (mL/min) | MMR (WU) |
|---|---|---|---|---|---|---|---|
| 1 | 0.98 | 2.0 | 18 | 0.93 | 0.93 | 159 | 605 |
| 2 | 0.93 | 2.6 | 14 | 0.89 | 0.78 | 112 | 830 |
| 3 | 0.96 | 2.9 | 40 | 0.86 | 0.82 | 117 | 823 |
| 4 | 0.98 | 1.7 | 25 | 0.93 | 0.84 | 160 | 351 |
| 5 | 0.94 | 3.2 | 11 | 0.91 | 0.83 | 180 | 444 |
| 6 | 0.97 | 4.4 | 20 | 0.99 | 0.99 | 130 | 632 |
| 7 | 0.94 | 1.3 | 34 | 0.96 | 0.88 | 108 | 667 |
| 8 | 0.96 | 2.5 | 10 | 0.86 | 0.83 | 176 | 464 |
| 9 | 0.91 | 1.2 | 13 | 0.91 | 0.92 | 201 | 411 |
| 10 | 0.96 | 2.1 | 28 | 0.76 | 0.81 | 115 | 653 |
| 11 | 0.97 | 5.1 | 9 | 0.84 | 0.84 | 190 | 253 |
| 12 | 0.96 | 3.6 | 12 | 0.89 | 0.81 | 179 | 266 |
| 13 | 0.90 | 1.4 | 28 | 0.89 | 0.87 | 101 | 718 |
| 14 | 0.98 | 4.4 | 15 | 0.88 | 0.80 | 147 | 675 |
| Mean | 0.95 | 2.7 | 20 | 0.88 | 0.86 | 148 | 557 |
AF, absolute coronary flow; CFR, coronary flow reserve; FFRa, fractional flow reserve induced with adenosine; FFRs, fractional flow reserve induced by intracoronary saline infusion; IMR, index of microcirculatory resistance; MMR, minimal microvascular resistance; Pd/Pa, ratio of mean intracoronary pressure to mean aortic pressure.
Our study confirms the ability of thermodilution with continuous infusion of room-temperature saline to quantify functional parameters of intracoronary blood flow in a population of patients with no angiographically significant coronary lesions. These quantified variables are obtained by the infusion of saline solution through a specially designed catheter. This new method is the first to allow quantitative measurement of MCF and minimal vascular resistance. A recent study confirmed that intra-arterial infusion of room-temperature saline solution can induce vasodilation in the absence of adenosine.3 However, until now there were no published data on MCF and minimal microvascular resistance in human patients. Further studies are needed to determine the normal values for these parameters and the implications of their alteration in different disease settings.