Keywords
INTRODUCTION
Bicuspid aortic valve (BAV) is the most frequent congenital heart defect (in 1%-2% of the general population).1 It is associated with the development of valvular and aortic wall disease, secondary to histopathological alterations known as cystic medial necrosis.2 Its form of presentation tends to change depending on age: aortic stenosis or endocarditis in children; aortic dissection and aortic regurgitation (AR) in young people; and aortic stenosis due to valvular calcification in adults.3
Aortic regurgitation in the presence of BAV has become one of the main surgical indications for severe AR in less than 50 years in our setting. Thus, most patients who require surgery for BAV failure are young people with long postoperative life expectancy. In these individuals, the implantation of artificial heart valves involves a high cumulative risk of complications (thrombosis, thromboembolic events, and hemorrhages). Valve-sparing surgery has been an attractive alternative to prosthetic replacement for many years. However, whereas mitral valve repair is a fully accepted and standardized procedure, acceptance of BAV repair, whether associated with ascending aorta disease or not, still has to overcome several problems. We present three cases illustrating different clinical situations, as well as the usefulness of echocardiography for describing the valvular anatomy.
METHODS
Case 1
Male, 21 years old, admitted for moderate effort dyspnea. Surgical treatment was diagnosed and prescribed for severe AR due to BAV. Intraoperatorive transesophageal echocardiography (TEE) was done confirming the presence of a BAV with flexible symmetrical leaflets, median raphe in the anterior leaflet, and prolapse of both leaflets in the left ventricular outflow tract (LVOT), with a central AR jet originating over the entire margin of coaptation between the 2 leaflets. The ascending aorta and aortic root were of normal dimensions, with appropriate proportions between the annulus and the sinotubular junction (STJ) (Table). Surgical repair was undertaken by resecting the median raphe, subcommissural annuloplasty, and free edge reinforcement of both cusps with Gore-Tex. Intraoperative TEE confirmed successful resuspension of both leaflets, with a residual eccentric grade 2 AR jet and a mean transvalvular gradient of 18 mm Hg at the cardiopulmonary the end of extracorporal circulation. Initially, the patient evolved satisfactorily, but echocardiographic study at 3 months after surgery showed severe AR recurrence without structural failure of the leaflets, with an eccentric jet directed toward the interventricular septum, another central jet, and anterior leaflet prolapse in the LVOT. The patient is currently waiting aortic valve replacement with an artificial heart valve.
Case 2
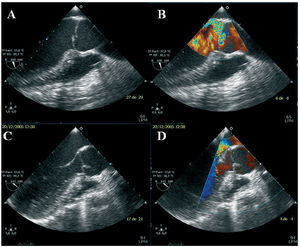
Male, 36 years old, admitted for aortic valvular surgery due to severe symptomatic AR. Transthoracic echocardiography showed a dilated left ventricle and severe AR due to BAV. Intraoperatorive TEE showed normal geometry of the aortic root and ascending aorta, although slightly dilated (Table), a BAV with flexible asymmetrical leaflets, thickening in both commissures, and anterior leaflet prolapse in the LVOT (Figure 1A). Aortic regurgitation was eccentric, directed toward the anterior leaflet of the mitral valve (Figure 1B). Repair was done via quadrangular resection, resuspension of the anterior leaflet, shaving the commissures, and subcommissural annuloplasty. Intraoperatorive TEE demonstrated successful repair, with both leaflets having a broad coaptation surface, the coaptation point remaining suitably high in relation to the aortic annular plane, and a central grade 1 AR jet (Figure 1C and D). The patient evolved well. Currently, he is asymptomatic and without anterograde systolic flow through the aortic valve or AR progression in the control echocardiography 6 months after surgery.
Figure 1. Intraoperatorive transesophageal echocardiography. A: aortic long axis showing lack of coaptation due to anterior leaflet prolapse. B: the color image reveals an eccentric jet, contralateral to the prolapsed leaflet. C and D: postoperative images showing the corrected defect and absence of residual aortic regurgitation.
Case 3
Woman, 28 years old, surgically operated for progressive dilatation of ascending aorta and symptoms (chest pain) attributable to the aneurysm, with AR due to BAV. Previously, imaging studies (thoracic computed tomography [CT] with and without contrast agent) had ruled out acute aortic disease while confirming the presence of a 5-cm (max. diameter) ascending aortic aneurysm (Table). Intraoperatorive TEE showed a BAV with symmetrical flexible leaflets, without calcification or thickening, with mild posterior leaflet prolapse in the LVOT. The AR (assessed as grade 3 by semiquantitative methods) was characterized by an eccentric jet directed toward the interventricular septum. It was decided to replace the ascending aorta with a Dacron tube graft and remodel the posterior sinus of Valsalva, which was macroscopically aneurysmatic, with resuspension of the same leaflet. At discharge, she presented grade 1 AR, stable at 5-year follow-up, during which she remained asymptomatic, without AR-grade progression being seen or dilatation of the aortic root residual tissue.
DISCUSSION
Aortic regurgitation due to BAV can be caused by commissural margin retraction, leaflet prolapse, aortic root dilatation, or valvular destruction secondary to endocarditis. It is technically possible to repair a BAV, with similar or even better results than in tricuspid aortic valve (TAV) repair. This is probably due to the high level of surgical skill necessary for reconstructing three coaptation lines in the TAV, compared to the relative simplicity of preserving a single line in the BAV.4 With minimum comorbidity,5 BAV reconstruction has shown even higher valve gradients at rest and with exercise than with prosthetic valves.6
In a retrospective study by Crosgrove et al7 in 75 individuals who underwent BAV repair, the following were predictors of successful repair:
1. Eccentric regurgitant jet direction due to leaflet prolapse.
2. Lack of cusp thickening and calcification.
3. Lack of commissural thickening or fusion.
Our first patient presented prolapse of both leaflets, a central AR jet over the margin of coaptation, and extensive median raphe thickening in the anterior leaflet which needed quadrangular resection, with a residual grade 2 AR before hospital discharge, which could explain the early failure of surgical repair. On the other hand, surgical repair has been effective in the medium term in the second case, with AR due to anterior leaflet prolapse, asymmetric leaflet size, and an eccentric regurgitant jet.
However, despite the early success of repair, the long-term prognosis is less encouraging. In a recently published study,8 at 1-, 5-, and 8-year follow-up, AR recurrence and need for reoperation were 3.2%, 11%, and 18%; and 5.3%, 29%, and 56%, respectively. Although the reason for repair failure is not well understood, some studies have found significant AR presence prior to discharge and aortic root abnormalities as predisposing factors for reoperation, being present in up to 50% of patients with BAV.9,10 In the follow-up study published up to the to date, structural failure of the aortic valve leaflets or progression to aortic stenosis have not been described as causes for reoperation.
It is well known that progressive aortic dilatation is an independent problem in valvular disease,2 that not only continues after the problem is solved, but seems to be a risk factor for AR recurrence and the need for second intervention in patients with valve repair or replacement.11,12
Current indications for ascending aortic replacement in patients with BAV (regardless of the need for simultaneous AR surgery) are:
1. Aortic diameter >5 cm.
2. Rapid growth in aortic diameter > 3-5 mm per year.
3. Symptoms attributable to the aneurysm.
4. Aneurysm of one or both sinuses of Valsalva.11
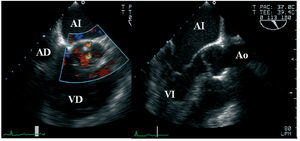
Decisions regarding when to carry out prophylactic aortic root replacement in patients undergoing surgery for AR continues to be controversial. In a study by Borger et al12 the aortic complication rate in patients with valve replacement at 15-year follow-up was 14%, 19%, and 57% when the aortic diameter was <4, 4-4.4, and 4.5-4.9 cm, respectively; therefore, prophylactic ascending aortic valve replacement was recommended when aortic diameter was >4.4 cm. Thus, the limited long-term durability of repair might have been due to aortic root dilatation not being taken into account at the time of surgery, which may occur during long-term follow-up in the second of our patients, whose aortic diameter was already at the limit of indications for surgery at the time of the intervention. In fact, some authors propose combining valve repair with root remodelling techniques when diameters are >33 mm at the STJ.13 Such new surgical techniques of aortic replacement combined with valve repair (Figure 2) seem to lead to more stable results (as in the last of our patients, who was free from AR or need for intervention after 5-year follow-up). Despite being technically more complex than valve repair alone, it is not associated with increased operative mortality and morbidity,13,14 thus, it could be a solution in patients with a specific degree of dilatation of the ascending aorta. In any case, it is worthwhile bearing in mind that every complex technique has a learning curve and that the published data come from centers experienced in this type of surgery.
Figure 2. Transesophageal study 3 years after aortic root remodeling surgery and bicuspid aortic valve repair. Aortic long axis showing a Dacron tube with molded neo-sinuses. Aortic root geometry has a normal configuration. A minimum residual regurgitation is seen in the short axis under color Doppler ultrasound. RA indicates right atrium; LA, left atrium; Ao, aorta; RV, right ventricle; LV, left ventricle.
In conclusion, valve repair in aortic regurgitation due to BAV is a technically possible therapeutic alternative in selected cases of isolated aortic valve prolapse with an eccentric regurgitating jet and leaflets without macroscopic structural injury. However, AR recurrence is a problem in medium- and long-term follow-up in these patients. The new aortic valve-sparing techniques with ascending aortic replacement lead to more stable surgical results when patient selection is appropriate and the procedures are done in centers with surgical experience in this regard.
Correspondence: Dra. P. Gallego.
Unidad de Ecocardiografía. Hospital Universitario Virgen Macarena.
Avda. Dr. Fedriani, 3. 41071 Sevilla. España.
E-mail: pastoragallego@teleline.es
Received May 23, 2006.
Accepted for publication August 2, 2006.