Keywords
INTRODUCTION
The use of the radial access for coronary angiography was first proposed by Campeau1 in 1989. A few years later, it began to be employed for angioplasty procedures and stent implantation. This technique enables the treatment of the same types of lesions as the femoral approach and, moreover, offers several advantages. It is associated with a very low incidence of vascular complications and allows early ambulation, which results in greater convenience for the patient and shortens the hospital stay.3,4
CASE REPORTS
Case 1
The patient was a 55-year-old man with metallic mechanical mitral and tricuspid prostheses. In July of 2004, he had a non-ST-elevation acute myocardial infarction (AMI) and underwent diagnostic catheterization via right radial artery involving a 6-F introducer (1 F=0.33 mm) without interruption of the anticoagulation therapy.
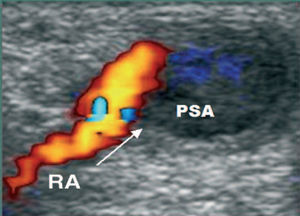
Two weeks later, he presented with a purplish, painful, throbbing mass at the site of the arterial puncture and systolic murmur which had appeared 24 hours after the catheterization. Doppler ultrasound revealed a pseudoaneurysm of the radial artery (Figure 1).
Figure 1. Ultrasound image of a radial artery pseudoaneurysm that developed after cardiac catheterization. The rounded, anechogenic image corresponds to the pseudoaneurysm (PSA), which communicates by way of its neck (arrow) with the radial artery (RA).
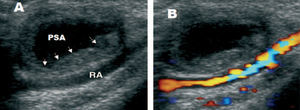
Mechanical compression was applied with elastic bands for 24 hours, with no improvement. A radial artery pneumatic compression device (TR Band®, Terumo) was subsequently employed for 72 hours, followed by an elastic bandage which was used for another 48 hours. Anticoagulation therapy was temporarily discontinued on the third day of treatment and, once the latter had been completed, the volume of the lesion was clearly reduced. A few days after anticoagulation was resumed, Doppler ultrasound was repeated and the cavity was seen to be partially thrombosed, with no connection to the arterial lumen (Figure 2). The outcome was favorable.
Figure 2. Ultrasound image of the thrombosed radial artery pseudoaneurysm after compression therapy. A: the lesion presents partial thrombosis in its peripheral zone (arrows). B: color Doppler echocardiography demonstrates the absence of flow in the residual lesion, which does not communicate with the underlying radial artery.
Case 2
This patient was a 57-year-old male smoker who, in July of 2004, had an acute anterior myocardial infarction. He underwent right transradial primary angioplasty, with implantation of 2 stents in the left anterior descending coronary artery. A 6-F hydrophilic introducer (Radiofocus® Introducer II, Terumo) was employed, without previous skin incision.
Two weeks after the catheterization, he presented with a purplish nodule measuring 1.5 cm in diameter at the site of the arterial puncture. A high-potency topical corticosteroid was applied and the size of the nodule was reduced after 7 days of treatment. The biopsy of the residual lesion disclosed a foreign-body granulomatous reaction surrounding a birefringent material (Figure 3).
Figure 3. A: photograph of the inflammatory lesion at the puncture site. B: microscope image of the biopsy showing epidermal hyperplasia and a fistulous passage that coincides with the catheter entry site. The underlying dermis presents a dense inflammatory infiltrate (HE, *40). C: high magnification microscope image showing a multinucleated giant cell (arrow), together with a birefringent foreign body (arrowhead) (HE, x400).
DISCUSSION
Pseudoaneurysm is an extremely rare complication of catheterization via radial artery.6,8 In their series, Sanmartín et al8 reported only 1 pseudoaneurysm among 3369 patients who underwent this procedure, in which a 6-F introducer was utilized and aspirin and clopidogrel, not anticoagulants, were administered. Complete resolution was achieved with 12 hours of compression bandaging.
A priori, the management of pseudoaneurysm of the radial artery should be easier than that of the femoral artery given that it is located in a smaller, more accessible artery that has a better underlying bone surface for compression. The poor initial response of our patient may have been due to the need for anticoagulation and perhaps to the delay in initiating treatment. This case suggests that it may be necessary to discontinue anticoagulation therapy in pseudoaneurysms of the radial artery that do not respond to initial compression. Pneumatic devices especially designed for this purpose, such as that utilized in our case, may also be useful.
The foreign-body granulomatous reaction to radial artery puncture typically occurs 2 weeks after the procedure, although it can develop a few days or months later. It disappears spontaneously and it has been speculated that tissue biopsy accelerates the resolution.7 In our patient, treatment with a topical corticosteroid resulted in a considerable reduction in the size of the lesion.
Kozak et al7 reported 33 cases of local inflammatory response after 2038 catheterizations using the radial approach (1.6%). The 10 lesions biopsied showed varying degrees of acute and chronic inflammation, and some of them presented a granulomatous reaction surrounding a grayish-blue extracellular material. The authors suggest 2 possible factors associated with this complication: the hydrophilic introducers (which increased the incidence to 3%) and the use of latex gloves (without which, the incidence decreased to 0.8%).
Hydrophilic introducers reduce patient discomfort during their introduction and withdrawal. Fragments that become detached from the hydrophilic coating may favor the development of a local inflammatory response, perhaps potentiated by the use of latex gloves (which are presently not utilized in our center). The powder on the gloves could adhere to the hydrophilic gel, forming a nidus for the inflammatory response.
Despite this circumstance, we consider that the advantages of hydrophilic introducers justify their use in radial artery access, since this complication is uncommon and benign.7,9 On the other hand, its incidence will undoubtedly be reduced by the progressive disappearance of latex gloves, the utilization of introducers with a smaller bore and the creation of an adequate skin incision with a scalpel blade, which facilitates the entry of the introducer and, thus, provokes less abrasion of the skin and underlying connective tissue.
Received November 25, 2004.
Accepted for publication February 3, 2005.
Correspondence: Dra. A. Blasco.
Unidad de Hemodinámica. Hospital Puerta de Hierro.
San Martín de Porres, 4. 28035 Madrid. España.
E-mail: alopezgf@telefonica.net