More and more patients with ischemic heart disease require dual antiplatelet therapy (DAPT).1 In patients undergoing a percutaneous coronary intervention (PCI) and stent implantation, DAPT use lowers the risk of stent thrombosis and adverse cardiac events, but hypersensitivity to aspirin greatly reduces the treatment options. Here, we report the long-term results of a series of patients with aspirin hypersensitivity who underwent coronary stent implantation and were treated with triflusal as an alternative to aspirin.
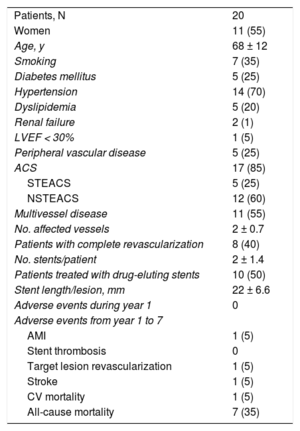
Between 2000 and 2013 in our center, 68 patients with ischemic heart disease had a history of hypersensitivity reaction to aspirin; 20% of them had undergone aspirin challenge testing. Among the total, 20 patients were treated with a PCI and stent implantation. At the onset of their condition, 17 patients (85%), had an acute coronary syndrome (ACS), 5 of them with ST elevation. Left ventricular systolic function was severely depressed (28%) in 1 patient, and was preserved in the remainder. A summary of the patients’ clinical characteristics is provided in Table.
Clinical Characteristics and Adverse Cardiac Events in Patients With a History of Aspirin Hypersensitivity Treated With a Coronary Stent and Dual Antiplatelet Therapy With Triflusal and a Thienopyridine
| Patients, N | 20 |
| Women | 11 (55) |
| Age, y | 68 ± 12 |
| Smoking | 7 (35) |
| Diabetes mellitus | 5 (25) |
| Hypertension | 14 (70) |
| Dyslipidemia | 5 (20) |
| Renal failure | 2 (1) |
| LVEF < 30% | 1 (5) |
| Peripheral vascular disease | 5 (25) |
| ACS | 17 (85) |
| STEACS | 5 (25) |
| NSTEACS | 12 (60) |
| Multivessel disease | 11 (55) |
| No. affected vessels | 2 ± 0.7 |
| Patients with complete revascularization | 8 (40) |
| No. stents/patient | 2 ± 1.4 |
| Patients treated with drug-eluting stents | 10 (50) |
| Stent length/lesion, mm | 22 ± 6.6 |
| Adverse events during year 1 | 0 |
| Adverse events from year 1 to 7 | |
| AMI | 1 (5) |
| Stent thrombosis | 0 |
| Target lesion revascularization | 1 (5) |
| Stroke | 1 (5) |
| CV mortality | 1 (5) |
| All-cause mortality | 7 (35) |
ACS, acute coronary syndrome; AMI, acute myocardial infarction; CV, cardiovascular; LVEF, left ventricular ejection fraction; STEACS, ST-elevation acute coronary syndrome NSTEACS, non–ST-elevation acute coronary syndrome.
Values are expressed as mean ± standard deviation or No. (%), unless otherwise indicated.
Half the patients received a drug-eluting stent. Patients were prescribed DAPT with triflusal 300 mg/12 h and 1 thienopyridine agent (clopidogrel, except in 3 patients with ACS and ST elevation, treated with prasugrel). None of the patients had a hypersensitivity reaction following triflusal administration. The duration of DAPT was 1 year in 18 patients (90%), 2 months in 1 patient with unstable angina treated with a conventional stent, and 6 months in 1 patient with concomitant oral anticoagulation treatment. Following completion of the DAPT period, 75% of patients continued treatment with triflusal indefinitely.
In the first year after the PCI, there were no cases of stent thrombosis or other adverse events. Mortality was 35% (7 patients) after a median follow-up period of 7.1 years. Only 1 patient died due to a cardiovascular cause: sudden death at 6 years following the intervention (Table).
There were no major bleeding events over the entire follow-up period. At more than 1 year following the PCI, 3 patients had experienced minor bleeding episodes (1 rectal bleeding and 2 hematuria).
In patients with aspirin hypersensitivity and ischemic heart disease requiring DAPT, aspirin desensitization is the solution recommended by most professionals. To date, several protocols described for this purpose have included ACS patients treated by stent placement.2 Nonetheless, aspirin desensitization may not always be possible: lack of resources at certain times (it must be done in an intensive care unit), clinically unstable patient, ongoing acute hypersensitivity reaction (asthmatic or angioedema), or a recent anaphylactic reaction.
Triflusal is a drug of the salicylate family that possesses a trifluoromethyl group, a characteristic that differentiates it from aspirin. In contrast to aspirin, triflusal inhibits cyclic adenosine monophosphate phosphodiesterase (cAMP) and cyclic guanosine monophosphate (cGMP). It is as effective as aspirin for inhibiting platelet cyclooxygenase 1 (COX-1), but it is able to maintain endothelial COX-2 expression levels.3 Triflusal has been mainly investigated in relation to peripheral vasculopathy or cerebrovascular disease; to date, the published results in cardiovascular disease are limited. In 1 multicenter study including more than 2000 patients, triflusal was not inferior to aspirin with regard to mortality, reinfarction, or the need for repeat revascularization in acute myocardial infarction patients.4 Furthermore, even though it is a member of the salicylate family, triflusal has proven to be safe for patients with aspirin hypersensitivity leading to exacerbation of respiratory disease.5 In a recent study including 127 patients with a history of aspirin intolerance or hypersensitivity, 8 patients (6.3%) were treated with triflusal and 1 with thienopyridine following implantation of a coronary stent. There were no cases of stent thrombosis during the time patients were receiving DAPT, and the infarction and mortality rate at 3 years of follow-up was 3.1%.6
In the present series of patients with aspirin hypersensitivity treated with a coronary stent, triflusal use was associated with low rate of adverse events at long term, and there were no cases of stent thrombosis in the first year or hypersensitivity reactions to triflusal.
The main limitation of this study is the small number of patients included. In addition, aspirin challenge testing to confirm hypersensitivity was carried out in only 20% of patients, a limitation related to the retrospective nature of the study.
The association of aspirin hypersensitivity and ischemic heart disease requiring DAPT is not common in our daily practice, but it could pose a problem for adequate treatment. If aspirin desensitization cannot be carried out, triflusal use seems to be a safe and effective alternative.