Keywords
INTRODUCTION
Etiological diagnosis of arterial embolisms is a complex task. Nonetheless, the emboligenic source can be identified in 90% to 95% of patients with noninvasive imaging techniques.1,2 Around 85% of peripheral arterial embolisms originate in the heart.2 Transesophageal echocardiography (TEE) is highly useful in this condition because it allows a thorough examination of both the heart and the thoracic aorta.1 The aorta is now generating increasing interest as a potential source of embolisms; it has been estimated that 5% of embolisms originate in the aorta.1 Thrombi mainly proceed from the abdominal aorta and adhere to aneurysms or arteriosclerotic lesions, although they have also been found in apparently healthy vascular segments. The presence of thrombi in the thoracic aorta is much less common, particularly when there is no concomitant aneurysm or atherosclerotic disease.3,4 The optimal treatment for these patients is not well defined.
The aim of the present study is to describe the clinical characteristics and evolution of 3 patients with peripheral arterial embolism, in whom thrombosis of the thoracic aorta was documented.
METHODS
Between September 2002 and July 2006, thoracic aorta thrombi were found in 3 patients admitted to our hospital for arterial embolism. The imaging modalities used in these patients included TEE, computed tomography (CT), and/or magnetic resonance (MR) imaging. All patients had a macroscopically normal aorta (no arteriosclerosis or aneurysms).
RESULTS
The characteristics of the study patients are described below and presented in Table 1.
Case 1
A 54-year-old man with hypertension and dyslipidemia came to the emergency room for sudden onset of pain in the right arm, which showed an absence of humeral pulse. A TEE was performed to exclude acute aortic disease. A mass was detected in the descending aorta, immediately distal to the left subclavian artery, and was interpreted as a flap from a dissection. Subsequently, arteriography additionally documented a filling defect in the ascending aorta, 3 cm from the aortic valve plane. The patient was diagnosed with type A aortic dissection and underwent surgery. During the postoperative period he experienced a massive stroke and died. Examination of the surgical specimen identified a thrombus adhered to a small atherosclerotic plaque in the ascending aorta. There was no dissection.
Case 2
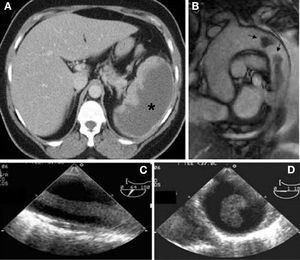
A 47-year-old woman with hypertension consulted for pain in the epigastrum and left hypochondrium. Abdominal-pelvic CT showed a massive splenic infarction (Figure 1). The transthoracic echocardiography (TTE) was normal and blood cultures were negative. TEE showed a large, highly mobile mass anchored in the aortic isthmus (Figure 1). The aorta was normal. Intravenous heparin was started, but the aortic mass persisted on subsequent follow-up studies. Hence, surgery was indicated and 2 masses were resected (Figure 2). Histological study confirmed their thrombotic nature. Hypercoagulability testing was normal.
Figure 1. Imaging studies (patient 2). A: abdominal computed tomography, axial view, shows a large, dense area in the spleen (massive splenic infarction) (*). B: magnetic resonance imaging, sagittal view of the ascending aorta, aortic arch, and proximal portion of the descending thoracic aorta; 2 high-density images (arrows) are observed in the aortic lumen, corresponding to aortic thrombi. C: transesophageal echocardiography, long-axis view of the descending thoracic aorta distal to the left subclavian artery; an echodense digitiform image is observed, corresponding to the most distal thrombus. D: transesophageal echocardiography, cross-sectional view of the descending thoracic aorta distal to the origin of the left subclavian artery, in which the thrombus is also evident.
Figure 2. Surgical specimen. A: macroscopic view of the irregular, heterogeneous, digitiform mass; the anchoring point is at the extreme right. B: cross sections at several levels of the thrombus, in which its heterogeneous nature is seen.
Case 3
A 52-year-old man, a smoker with hypercholesterolemia and hypertension, came to the emergency room for pain in the right iliac fossa, vomiting, and diarrhea. The abdominal CT scan showed signs of ileitis, left kidney infarction, and massive splenic infarction. Blood cultures were negative. The TTE and TEE findings ruled out a cardiac origin. TEE detected a pedunculated mass anchored in the aortic isthmus. The aortic wall had a normal appearance. The patient was started on heparin anticoagulation and was scheduled for surgery. On an MR imaging study performed before surgery the thrombus was seen to have disappeared. Thrombophilia testing was negative.
DISCUSSION
We present 3 patients with arterial embolism and thrombosis of a thoracic aorta with an apparently normal wall. Several series of patients with thoracic aorta thrombi have been reported (Table 2).1-7 Our patients share some important features with the reported cases, but also present some peculiarities.
The most frequent clinical presentation is embolism of the limbs, with a certain predilection for the left arm.7 This clinical presentation was seen in patient 1 of the present study, although the affected limb was the right arm. The other patients presented with a visceral embolism. This is an uncommon location that was seen in only 5 patients among those included in the above-mentioned series. On occasion, there are multiple embolisms (10% of patients at the time of clinical presentation in the largest series6). In our series, patient 3 presented with several embolisms and all were located in the viscera.
The most frequent location of thoracic aorta thrombi is the region of the aortic isthmus and the portion distal to the aortic arch, at the side opposite to the origin of the subclavian artery.7 All our patients had thrombi in this region and in patients 1 and 2, more than one thrombus was detected. In patient 1, one of the thrombi was in the ascending aorta, which is the most uncommon location.
The pathophysiology of aortic thrombi is not well -defined. They occur more commonly in patients of advanced age and those with several cardiovascular risk factors and severe aortic atheroscleriosis,1,6 although they have also been described in apparently normal aortas and in those with circumscribed arteriosclerosis at the site where the thrombus is anchored to the vessel. The mean age of our patients was 51 years, and except for the third case, they had a low cardiovascular risk profile. In some series,4 aortic thrombosis was accompanied by chronic inflammatory disease, which was absent in our patients. Hypercoagulability testing was negative in all 3 patients, a frequent finding in other reported series.2,6,7
The differential diagnosis of aortic thrombi must be established with other aortic masses, such as tumors.8 The definite diagnosis requires histological and immunohistochemical studies, but MR is the most useful imaging test for the differential diagnosis.8 The differential diagnosis with aortic dissection is also important because of the therapeutic implications. TEE may be better than other imaging techniques applied for this purpose, particularly CT.9
The most widely used technique in the diagnosis of aortic thrombosis in the reported series is TEE. This test has high diagnostic accuracy and allows assessment of the size, morphology, and anchoring site of the thrombus, as well as the characteristics of the aortic wall. Although there are no studies comparing the various imaging techniques in the diagnosis of aortic thrombosis, it is likely that they have similar diagnostic accuracy, as occurs in other diseases of the thoracic aorta.
There is general consensus that these patients should receive anticoagulation therapy.1,2,4-7 Surgical treatment (thrombectomy) is reserved for selected cases of recurrent embolism or persistent thrombus despite proper anticoagulation. As occurred in our third patient, complete resolution of the thrombus has been described following anticoagulation therapy.2,7 Some authors recommend TEE in the 24 h prior to surgery to confirm persistent thrombus.7 All our patients with the exception of patient 1 (in whom dissection was suspected initially) received anticoagulation with heparin sodium. In patient 2, thrombectomy was performed after anticoagulation treatment had failed.
The prognosis of these patients is mainly determined by the consequences of the embolism. In our series, 1 patient died due to a massive cerebral embolism. The clinical evolution of the other 2 patients was favorable, and there was no evidence of recurrence in the follow-up.
In patients with arterial embolism, it is advisable to investigate the thoracic aorta as the possible source in addition to the typical embolic foci, even in patients without classic cardiovascular risk factors.
Correspondence: Dr. I. Vilacosta.
Instituto Cardiovascular. Hospital Universitario San Carlos.
Prof. Martín Lagos, s/n. 28040. Madrid. España.
E-mail: ivilac@medynet.com
Received March 8, 2007.
Accepted for publication July 19, 2007.