Keywords
INTRODUCTION
Chagas disease is the leading cause of infectious myocarditis,1 which affects 30% of the 10 million infected persons in Latin America,2 distributed over a wide geographical area between the latitudes of 42° North and 40° South.
The estimated incidence of 700 000 new cases per year fell to fewer than 200 000 cases per year in 2000.3
The pathogenesis of chronic Chagas heart disease has not been fully established,4 although possible mechanisms of the progressive myocardial damage8 include the persistence of the parasite in the myocardium5-7 and the specific abnormalities of the host immune response, which cause chronic myocarditis that evolves to cardiac fibrosis.9
The diagnosis of Chagas disease during the indeterminate and chronic stages is based on the detection of specific antibodies to Trypanosoma cruzi using serologic tests (immunofluorescence test, indirect hemoagglutination, and enzyme linked immunosorbent assay—ELISA). The diagnosis should be confirmed by at least 2 different reactive serologic tests in order to avoid false positive results. The complete negativization of the serology is the main criterion for a cure10 and a prognostic indicator of a favorable course for patients with the disease,11 together with other prognostic indicators such as the etiologic treatment, whereas cardiac conduction disorders or bundle branch block, older age, an increase in left ventricular systolic diameter and sustained ventricular tachycardia are clinical predictors of progression of the cardiomyopathy.12
Chronic Chagas disease may lead to the development of heart disease in 30% of affected persons, whilst 70% will later have no symptoms of the disease. Nevertheless, the slow course of chronic myocarditis has led to the idea that those patients without symptoms are in fact in an indeterminate stage of the disease, as they may or may not develop heart disease. Thus, the concept of progression refers to the observation of a change over time in the clinical state of the patient to another more severe state.
Although numerous prognostic indicators are known from the clinical point of view,13 no studies have yet been carried out concerning the importance of the socioeconomic conditions of the host as determinants of the persistence or control of chronic Chagas disease. Socioeconomic indicators have been investigated for other cardiovascular diseases, with diverging results4; some authors consider them to be risk factors.
The aim, therefore, of this study was to evaluate, in patients with chronic Chagas disease, the impact of socioeconomic conditions on the serologic evolution, by the observation of negative seroconversion, and the clinical evolution, using indicators of the progression of the heart disease, during prolonged follow-up of these patients.
METHODS
Study Population and Variables
Out of a total of 1177 patients attended at a referral center in Argentina between 1990 and 2005, the study included 801 patients with chronic Chagas disease and hospital outpatient follow-up. A full clinical history was taken on admission, including data on the following socioeconomic variables: birth in rural endemic area, time of residence in endemic and urban areas (in years), overcrowding index (ie, number of inhabitants divided by the number of rooms, excluding kitchen and bathroom), absence of toilet facilities, years of education or study, employed or unemployed, and health insurance coverage (ie, private contributory medical insurance coverage).
The socioeconomic variables were based on the indicators of non-satisfied basic needs of the National Census and Statistics Institute of the Argentine Republic, used by many other authors in developing countries.15-19
Inclusion Criteria
As we wanted to study the serologic evolution of the disease, the study only included patients with 3 serologic tests that were reactive for Chagas disease (indirect hemoagglutination, immunofluorescence, and ELISA) carried out at the Dr Mario Fatala Chaben National Parasitology Institute reference center.
On admission, the patients were grouped according to their symptoms using the Kuschnir classification20: group 0, positive serology, normal electrocardiogram (ECG), and chest radiography with a cardiothoracic index (CTI) <0.50 (with no cardiomegaly); group I, positive serology, abnormal ECG,11 and chest radiography with CTI<0.50 (with no cardiomegaly); group II, positive serology, abnormal ECG, and chest radiography with CTI>0.50 (with cardiomegaly), with no signs or symptoms of heart failure; group III, positive serology, abnormal ECG, and chest radiography with CTI>0.50 (with cardiomegaly), with signs or symptoms of heart failure.
All the patients with radiologic cardiomegaly underwent an echocardiogram to confirm left ventricular dilatation, defined as such when the diastolic diameter was >57 mm (normal value in our service).
Exclusion Criteria
Patients were excluded from the study if they had a diagnosis of diabetes, alcoholism (average consumption of more than 100 g of alcohol per day for at least 10 years), autoimmune disorders, cancer, or other diseases that could shorten life expectancy (senile dementia, hemiplegia, hepatic cirrhosis, chronic renal failure, etc.) (202 patients).
The reason for these exclusions was the possibility that these comorbidities might modify the prognosis in a longitudinal study21 and also affect the immune system, thereby influencing the antibodies to be measured in the serologic tests.
Patients were also excluded if they were younger than 18 years of age (n=67), if they had not completed all the studies on admission (n=27), or if they only had 2 positive serologic tests (n=80).
Etiologic Treatment
Etiologic treatment with benznidazole, 5 mg/kg/d for 30 days, was indicated by agreement between the physician and the patient during the first month of follow-up: 373 patients received this treatment (47%).
Follow-up
The serology was repeated every 3 years during the follow-up, whereas the ECG and the chest radiography were repeated annually to group the patients clinically. The results were analyzed for all 801 patients included, and the follow-up was concluded in December 2008.
Evaluation Outcome Measures
The primary endpoint to evaluate the impact of the socioeconomic variables was negative seroconversion, defined as negative results on at least 2 of the 3 serologic tests in patients with 3 positive reactions on admission. The follow-up time for the serology was determined in the patients with a negative result, as well as for those with persistent positive tests.
The secondary endpoint was the change in clinical group (Kuschnir) to one of greater severity during the follow-up, considered to be a marker of progression of the heart disease.
Statistical Analysis
The continuous variables are presented as averages and the standard deviation (SD) or medians (25%-75% interquartile range) and the categorical variables as percentages of the total. The Kolmogorov-Smirnov test was used to explore the normal distribution of the continuous variables. One-way analysis of variance, the χ2 test and the Kruskal-Wallis test were used to test for differences between the clinical groups at admission, according to whether they were continuous numerical variables with a normal distribution, categorical variables or numerical variables with a non-Gaussian distribution, respectively. The correlation between the different socioeconomic variables was studied using Spearman's correlation test. Cox proportional risk regression was used for the univariate and multivariate analyses, calculating the hazard ratio (HR) and the 95% confidence intervals (CI) for each socioeconomic variable and the evaluation endpoints.
All the variables with P<.10 in the Cox univariate model were included in the multivariate model. A Cox proportional risk regression model was applied for each socioeconomic variable, without finding any violations of the suppositions of the model (overfitting, independence of the observations, and no crossing of the Kaplan-Meier curves). The variable "years of study" was transformed into a dichotomous variable (complete or incomplete primary studies) and represented by a Kaplan-Meier curve. All reported P values were 2-tailed and a P<.05 was considered significant.
The study protocol was approved by the institutional Ethics and Research Committee and the patients gave verbal consent for inclusion. The confidentiality of all the data was respected.
RESULTS
Baseline Characteristics
Table 1 shows the baseline characteristics of the patients with chronic Chagas disease, according to their clinical group on admission. The mean (SD) age was 42.2 (12.9) years, 57% were women and 43% men. More than half the patients had symptoms, mainly palpitations (27%) and atypical precordial pain (24%), whilst 34% presented a specific anomaly on the ECG (67% of them, conduction disorders). The conduction disorders found (181 patients) were: complete right bundle branch block (CRBBB), 56/181 (31%); left anterior hemiblock (LAHB), 42/181 (23%); CRBBB + LAHB, 59/181 (33%); incomplete right bundle branch block + LAHB, 22/181 (12%); and complete left bundle branch block, 2/181 (1%). The ventricular arrhythmia complexes were: polymorphic ventricular extrasystole (10 cases), ventricular pairs (12 cases), unsustained ventricular tachycardia (1 case), and sustained ventricular tachycardia (2 cases).
The distribution according to clinical group using the Kuschnir classification20 was predominantly (90%) groups 0 and I (with no heart disease or mild heart disease). All the variables related with the severity of the heart disease, such as ECG disorders, echocardiographic diameters, and left ventricular aneurysms, as well as age and sex, showed a relation with the clinical grouping (Kuschnir). The patients with more advanced heart disease at the time of admission came mainly from the geographical area situated between latitudes 28o S and 32o S in the endemic area. Other baseline socioeconomic characteristics, such as living in precarious housing (no doors or windows, walls of adobe, and roofs of straw), time of residence in the endemic area, overcrowding index, years of study, employment and medical insurance coverage also showed a relation with the severity of the cardiomyopathy. The median follow-up of the study was 10 years (25%-75% interquartile range, 7-14) and the average number of serologies per patient during the follow-up was 3. During the study, 62 (8%) patients were lost to follow-up.
Correlation Between the Socioeconomic Variables
Table 2 shows that there was a multiple correlation between the socioeconomic variables (multicolinearity), reflecting similar aspects of the same condition of the patients (the socioeconomic level). Accordingly, we decided to analyze them separately.22,23
Serologic Negativization
Of the total of 801 patients, 535 (67%) continued having 3 positive serologic tests and 155 (19%) showed negative seroconversion of 2 or 3 tests. Negativization of 1 test was seen in 111 (14%) patients.
The mean "serologic" follow-up period of the patients who became negative in 2 or 3 tests was 11.1 (5.2) years, whereas in the patients who continued having 3 positive tests this period was 10.3 (5.3) years, differences that were not statistically significant.
The variables with differences (P<.10) in the univariate Cox analysis were included separately in a Cox multivariate model, adjusted for age and etiologic treatment (Table 3).
Negative seroconversion of the serologic tests (best serologic evolution) was related with the following socioeconomic variables: less time living in an endemic area, a lower overcrowding index, and medical insurance coverage, whereas more years of education showed an almost significant trend.
Changes in Clinical Group
A change in clinical group (a marker of clinical progression of heart disease) was more usual in patients with 3 positive serologic tests (64/538, 12%) than in patients with negativization of 2 or 3 serologic tests (18/263, 7%) (P<.03).
Mortality during the follow-up of the 801 patients with chronic Chagas disease was 2% (16 patients): 1/505 (0.2%) in group 0 (pancreas cancer); 5/227 (2.2%) in group I (pneumonia, leukemia, heart failure, and 2 stroke); and 10/69 (14.5%) in groups II and III (6 heart failure and 4 sudden death).
The results of the Cox univariate and multivariate analyses for changes in clinical group (secondary endpoint) are shown in Table 4. There was a greater percentage of disease progression in the patients with advanced heart disease (groups II and III), less in the patients with mild heart disease (group I) and the lowest percentage in the patients with no initial heart disease. The clinical adjustment variables for the multivariate analysis (age, sex, ECG abnormalities, and etiologic treatment) showed differences (P<.10) in the univariate analysis, according to the previously described method.
The absence of toilet facilities, time of endemic and urban residence, overcrowding index, occupation and birth in an endemic area showed no significant differences in relation to the changes in clinical group.
Considering the subgroup of 697 patients with echocardiographic data, another Cox regression model was constructed to evaluate predictors of changes in clinical group, adjusting each socioeconomic variable for age, sex, ECG abnormalities, etiologic treatment, left ventricular diastolic diameter (LVDD), and left ventricular systolic diameter (LVSD), with similar results for the socioeconomic variables, presented in Table 4: left ventricular diastolic diameter (HR=2.65 [1.87-3.74]; P<.001); left ventricular systolic diameter (HR=2.16 [1.63-2.87]; P<.001); years of education (HR=0.87 [0.78-0.97]; P=.009); and medical insurance coverage (HR=0.45 [0.27-0.77]; P=.003).
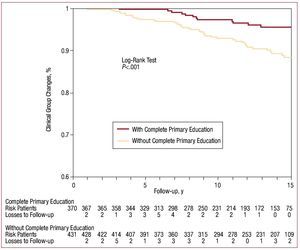
Figure 1 shows the differences in the Kaplan-Meier curves for the patients with complete or incomplete primary education.
Figure 1. Kaplan-Meier curve of the accumulative percentage of patients with changes in the clinical group with and without complete primary education (1990-2008).
Finally, access to medical insurance and a greater number of years of education were associated with a reduction in the likelihood of progression to heart disease, independently of the clinical adjustment variables.
DISCUSSION
Chagas disease develops within a socioeconomic context of poverty, present unfortunately in developing Latin American countries. The true prevention (the elimination of the transmission vector) and control of Chagas disease will probably continue depending on the economic, political and social future of Latin American countries.24
Most persons with Chagas disease have a low income and poor health and nutrition conditions, as well as very few opportunities for education or obtaining adequate housing. This poverty not only restricts access by the patient to the diagnosis and treatment of the disease, but it also leads to malnutrition and conditions the educational and working future of these persons.25,26 As well as the biological problem of Chagas disease, consideration should be given to its social dimension, which influences the health / disease process. Psychoneuroendocrineimmunology studies the strong social influences on the biology of each person, and in Chagas disease the clinical course depends on the social dimension as well.27
The presence of the parasite and the host immune response to eliminate it seem to be key in chronic Chagas disease. Negativization of the serology, used as the primary evaluation endpoint in this study, is the main criterion for cure. As well as the presence of the parasite, other factors can play a role in the evolution of infected patients and determine their state of health or disease. Nutritional, psychological and stress factors all related with the socioeconomic conditions could be important when determining the efficacy of the immune response in chronic diseases.28 The immune system can control the infection and prevent the appearance of Chagas disease, or even achieve a spontaneous cure.11,29,30 A deficient immune cell response against the antigens of T cruzi in symptomatic patients, as opposed to those in the indeterminate phase, can indicate a relation between the immune system and disease progression.31
Negative seroconversion has been shown to be a clinical indicator of a favorable course in patients with chronic Chagas disease.11,24,30 The concordance between a shorter time of residence in an endemic area and a better serologic evolution could indicate a lower rate of reinfections and a lower "parasite load" among those persons who remain fewer years in their endemic habitat, as well as the possibility of reinfection with different parasite strains and the pathogenic interaction between these in persons who remain more years in an endemic area.
Migration to cities can favor better conditions of health care and work, and thus a better income than in an endemic area. Socioeconomic factors have been considered to be important for the development of various diseases.32,33 Traditionally, the indicators of socioeconomic status are education, occupation, income, and material wealth.34 Income and material wealth are difficult to quantify in persons who have Chagas disease if they are poor, unemployed, or in temporary jobs.35 Alternative indicators of economic status that are used include housing conditions, such as the toilet facilities and the overcrowding index, which are easy to evaluate and are of great importance in the population in developing countries.36 The overcrowding index and medical insurance coverage proved to have an independent value for negative seroconversion, and these are variables that mainly reflect economic status.
The degree of education has also been considered to be a very useful indicator of health37 and in Chagas disease it should be considered as part of the health care program.38,39
Notably, more years of study had a borderline significance for a favorable serologic evolution (perhaps due to the homogeneity of the low educational level) and, conversely, those patients with less education and those who lacked health care coverage had an increased risk of progression of the heart disease. The lack of medical benefits can mean it is impossible to obtain health care and adequate treatment, which then results in an adverse clinical course of the disease.
One limitation of this study concerns the absence of data on income and material wealth of the participants. Another limitation is the composition of our sample based on a cohort of patients on hospital follow-up. Nevertheless, it is opportune to remark that the results obtained were independent of the etiologic treatment with benznidazole and other clinical variables, which reinforces the importance of the socioeconomic conditions in patients with Chagas disease and persistent infection.
CONCLUSIONS
The socioeconomic conditions had a significant impact on the evolution of chronic Chagas disease, independently of the treatment and the clinical characteristics of the patients.
SEE ARTICLE ON PAGES 1211-6
Correspondence: Dr. R.J. Viotti.
José Hernández 3440. Villa Ballester (1653). Buenos Aires. Argentina.
E-mail: rviotti@arnet.com.ar
Received April 5, 2009.
Accepted for publication June 30, 2009.