Keywords
INTRODUCTION
Spontaneous coronary artery dissection (SCAD) is a rare cause of acute coronary syndrome (ACS).1 It mainly affects women who have few cardiovascular risk factors and its diagnosis has increased as the use of coronary angiography has expanded. SCAD is the separation of 2 of the 3 arterial wall layers,1 creating a false lumen2 whose progression can impair distal coronary blood flow and cause ischaemia, with various presentations ranging from elevated cardiac markers and ST without pain to sudden death.1 Our understanding of this syndrome is limited to a few isolated case reports and some small series and therefore its treatment and prognosis are not well established.3
METHOD
We analysed 19 cases of primary SCAD diagnosed in a tertiary hospital from May 1998 until January 2009. In this period, our centre performed 9502 angiograms on patients with ACS, which has increased considerably in the last 5 years. This is a descriptive study with follow-up.
RESULTS
The epidemiological characteristics of the series are shown in Table 1, while the individual breakdown of clinical presentation and the subsequent course of the disease are shown in Table 2. All cases in which ST elevation was documented underwent fibrinolysis or were entered into a primary angioplasty programme at our center, despite the fact that stent implantation was rejected (considered a conservative posture in the Table).
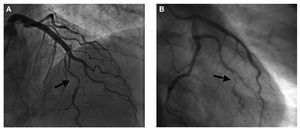
One of the cases appeared 2 days after uncomplicated vaginal delivery and 3 cases occurred in athletes after exhausting physical exertion (24-48 hours after exertion, with 2 of these cases after having run a marathon). Intense stress during the previous 24 hours was noted in 5 cases, and 7 of the cases occurred in patients taking estrogen (3 for oral contraception and 4 for perimenopausal hormone replacement therapy). The presence of autoantibodies was ruled out (in all cases: ANCA, ANA, and anti-DNA; in cases occurring in the last 5 years also anticardiolipin). No arteriosclerotic lesions were detected at other levels in the coronary angiographies (Figure 1). On 3 occasions, the diagnosis was confirmed using intravascular ultrasound.
Figure 1. Diagnostic coronary angiographies. A: spontaneous coronary sissection of the anterior descending artery in postpartum (case 6). B: typical narrowing of coronary dissection in a distal segment of the first marginal branch of the circumflex artery (case 8).
The first case in the series deserves special attention: a 47-year-old woman whose sister had spontaneous dissection of the internal carotid artery presented 2 SCAD (case 1 and 2 of the series). The first episode occurred 24 hours after running a marathon, and she was on oral contraceptives at the time. The patient presented with midthoracic tightness accompanied by intense vegetative symptoms. The emergency team determined anterior ST elevation and she underwent fibrinolysis. The following day, a catheterization was performed that revealed an anterior descending artery dissection in the middle segment and, due to her clinical stability, conservative treatment was chosen. Four years later, the patient still practiced sports regularly and had stopped taking contraceptives. Being on duty and after having treated a youth suffering from cardiorespiratory arrest, the emergency service attended to her. She presented similar symptoms with a new ST elevation, this time lower, and with an incomplete response to the initial fibrinolysis. In the subsequent catheterization, a proximal right SCAD was observed and a regular stent was implanted. The previously affected descending anterior artery did not have angiographic disorders this time around.
None of the patients underwent heart surgery and they were all discharged with preserved ejection fraction and given aspirin, beta-blockers and angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists as part of their treatment.
During outpatient follow-up, there were no cardiovascular events, regardless of treatment, except in the previously mentioned first case and no subsequent collagenopathies or neoplasias that might have been related to these events were diagnosed. The cardiologist who monitored each patient decided the long-term treatment unilaterally. Long-term use of aspirin was prescribed for cases with stent implants and for one case that later developed diabetes; beta-blockers were prescribed for 14 patients and low-dose statins were prescribed for 9 patients.
The patient in case 8 became pregnant and gave birth to a healthy baby who was delivered vaginally without complications two years after the dissection. The patient discontinued oral contraceptives and smoking after the heart attack and now engages in sports on a regular basis and is so far symptom-free.
DISCUSSION
SCAD is a rare disorder involving the dissection of the coronary wall, usually between the intima and the media (in cases involving atherosclerosis) or between the media and the adventitia (mostly in cases associated with childbirth). Ever since the first case was diagnosed in 1931 there have been over 300 published cases, many from autopsies performed after sudden death.2 The data are consistent with those of our series: more than 70% of those affected are women, 30% of cases are related to pregnancy, the anterior descending artery is affected in more than half of the cases and, once the acute phase is overcome, SCAD has a good long-term prognosis.3
The pathophysiology is not fully understood and has been associated with the inflammatory rupture of atherosclerotic plaques. In cases related to childbirth and/or postpartum, pericardial eosinophilic infiltrates have been reported during autopsies.2,4 This could be related to the effect of oestrogen and progesterone stimulating the esinophilic secretion of granules with lytic substances.4 This may also occur as a consequence of female hormonal treatments, which have already been associated with this problem.1,2
Other factors related to SCAD include hypertension,5 cocaine use,2 coronary spasms due to increased shear forces in the vessel,2 vasculitis,6 syndromes that present with abnormalities in the vascular walls (e.g., Marfan7), treatments such as cyclosporine2 and coronary compressive forces secondary to intramyocardial pathways and exhausting physical exercise.8 It is worth mentioning that there is a possible hereditary factor at play that could explain the reported familial groupings,9 such as with the first patient in our series.
Widespread use of coronary angiography in ACS has increased the number of diagnosed cases. An intimal flap is often observed, appearing as a radiolucent line that separates the double lumen along with indirect signs of dissection, such as the retention of contrast in the false lumen related to stenosis (Figure, A).3 Less often, we find arterial narrowing with no evidence of a flap, when there is no contrast flow in the false lumen (Figure, B). If in doubt, intravascular ultrasound10 and, even in the initial stages of implantation, optical coherence tomography11 can assist with a definitive diagnosis, especially when it is necessary to verify that the guidewire is in the true lumen before proceeding with the intervention. Coronary computed tomography12 can also help clarify the diagnosis non-invasively, especially when complications are suspected.
Treatment regimens depend on the location of the dissection, its accessibility and extent, the severity of the ischaemia and patient stability.2 The decision should be made on a case-by-case basis. For stable patients, those with only a small affected vessel or those whose affected vessel is in a location that precludes intervention, conservative medical therapy should be chosen. This happened in more than half of the cases in our series and is supported by the spontaneous resolution of the dissection during follow-up, as occurred in our first case. In patients with ischemia, especially those with severe affectation near a vessel, percutaneous intervention with direct stent implantation is recommended. For cases of multivessel disease and particularly when the left main trunk is affected, cardiac surgery may be the therapy of choice. There are reported cases where trunk dissection has been conducted successfully and conservatively.13
Fibrinolysis is not recommended due to risk of increased bleeding in the heart wall and advancing the dissection.1,3 Fortunately, it is applied less and less often as primary angioplasty programs are available 24 hours a day.
Full English text available from: www.revespcardiol.org
Correspondence: Dr. N. Romero Rodríguez.
Servicio de Cardiología. Hospital Universitario Virgen del Rocío. Avda. Manuel Siurot, s/n. 41013 Sevilla. Spain
E-mail: niemed21@hotmail.com
Received May 7, 2009.
Accepted for publicationSeptember 2, 2009.