The number and type of percutaneous catheterization techniques used for structural heart disease have exponentially increased in recent years. Diverse imaging techniques play fundamental roles before, during, and after these procedures.10.1016/j.recesp.2017.10.003
For transcatheter aortic valve implantation (TAVI), 2017 began with the publication of the 5-year echocardiographic follow-up of the PARTNER-I study,1 which confirmed the mid-to-long-term durability and stability of hemodynamic parameters after this procedure. Computed tomography (CT) continues to show superior reproducibility and ability to determine prosthesis size and the degree of its oversizing. In addition, during the postimplantation follow-up, CT is essential for detecting subclinical prosthetic thrombosis (areas of hypoattenuation in the prosthetic cusps), with an approximate incidence of 14.3%, which was not associated with increased prosthetic gradients or embolic events.
The field of percutaneous mitral valve interventions is expanding to include new devices aimed at repairing the valve using neochord implantation, rings, and edge-to-edge plication, together with the development of percutaneous mitral prostheses. The role of imaging in indication evaluation and monitoring has been strengthened. Publications from 2017 were oriented at identifying prognostic indicators based on percutaneous repair outcomes. A notable work by Neuss et al.2 reported worse 2-year vital prognosis for patients with a mean residual gradient > 4.4mmHg by echocardiography (or 5mmHg using invasive measurement), with a significant difference in the number of clips implanted per patient (1.3 vs 1.5 in the stenotic group). Regarding tricuspid valve interventions, the year began with multiple new repair systems and promising results. Because echocardiographic analysis of the tricuspid valve is poorly established, various groups have published recommendations on imaging analysis of the so-called forgotten valve. Another standout is the work by Hahn,3 with an excellent interventional cardiology-focused evaluation of the functional anatomy of the tricuspid valve.
Regarding periprosthetic leaks, an expert consensus was published in 2017 that includes recommendations for the quantification and characterization of periprosthetic leaks with multimodality imaging.4 In addition, the results were presented of a real-life Spanish clinical practice registry that shows the reliability and safety of the procedure.
In the field of left atrial appendage closure, one particularly pertinent article used various imaging techniques to show a significant intraprocedural increase in atrial appendage size after volume loading, with 3-dimensional echocardiography the most accurate technique for gauging the correct size of the device.5 In addition, prospective data from clinical practice, with more than 1000 patients treated with the Amulet device and 3-month echocardiographic follow-up in more than half of the patients, revealed a high rate of appendage occlusion (98.2%) with low rates of device thrombus (1.5%) in follow-up.
For percutaneous closure of the patent foramen ovale, the main contribution in 2017 has been the presentation of the preliminary results of the GORE-REDUCE study (NCT00738894), which showed the superiority of percutaneous occlusion over medical treatment in secondary prevention for patients younger than 60 years with septal aneurysm and a large defect, with echocardiography used to select ideal candidates. These results will probably be incorporated into the next guidelines.
Regarding congenital heart diseases, recommendations were published in 2017 on the value of 3-dimensional echocardiography,6 found to be particularly useful in the study and closure of abnormal and multiple communications or residual defects after surgery.
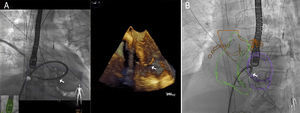
Good results in structural catheterization can be obtained with precise monitoring of the procedure. In contrast, the use of a transesophageal probe for more than 60minutes has been associated with an increase in oropharyngeal lesions, which may be indicated by an increased peripheral blood leukocyte count. A promising alternative is the transnasal probe, which, in addition to avoiding the need for general anesthesia, has shown good anatomical quality in various procedures. Fusion imaging (Figure) also safely reduces the procedural time and has become the best approach for transseptal puncture; for atrial appendage closure, fusion imaging with CT has also been shown to reduce the procedural contrast volume and time. Another emerging technology, especially suited to preprocedural planning, is 3-dimensional printing. Various articles have reported its ability to predict residual leaks after TAVI, test the safety of novel procedures, take accurate measurements and reduce the radiation dose in atrial appendage closure, and print material with different textures in the mitral valve field.
.