Keywords
INTRODUCTION
Reperfusion strategies in ST-segment elevation acute myocardial infarction (STEAMI) remain controversial.1 The earlier fibrinolysis is administered, the more efficient it is.2
Guidelines on STEAMI3 recommend door-to-needle times of <30 min for fibrinolysis and door-to-balloon times of <90 min for primary angioplasty. Analysis of the real-life context reveals time to myocardial reperfusion continues to exceed recommendations.4
The main objective of the present study is to analyze the influence of a new protocol to facilitate rapid identification of patients with STEAMI and thus reduce time to reperfusion, bringing it closer to guideline objectives. The secondary objective is to analyze intrahospital and 1-year prognosis before and after introducing the new protocol.
METHODS
On February 1, 2004, the chest pain service—located in the emergency room (ER) at a point as near as possible to the patient and ambulance entrance—became operational. It consisted of a an electrocardiogram (ECG) and a defibrillator, in order to conduct early ECGs on patients attending for chest pain, independently of angina type. If ST-segment elevation is identified, the duty cardiologist is called immediately to decide on the reperfusion strategy; if ST-elevation is not identified, patients are reclassified at a lower level of priority.
Between January 20, 2002 and January 31, 2004, 134 consecutive patients with STEAMI were admitted to the coronary care unit (CCU). Between February 1, 2004 and February 1, 2006, 161 consecutive patients with STEAMI were admitted. We prospectively recorded time to reperfusion and analyzed baseline characteristics and clinical course. We compared time to reperfusion in patients who received fibrinolysis before (group 1) and after (group 2) introducing the chest pain service. We evaluated intrahospital and 1-year prognosis in both groups, analyzing readmissions for cardiovascular cause, revascularization, non-fatal reinfarction, and cardiovascular death.
The reperfusion therapy used with most patients was fibrinolysis as our center has had a cardiac catheterization laboratory since June 2003. Consequently, we focus on the analysis of door-to-needle time, from arrival at ER to fibrinolysis. We briefly mention cases of primary angioplasty in the series, without considering their clinical course.
Statistical Analysis
We used SPSS® 12.0 for Windows for statistical analysis. Continuous quantitative variables with a normal distribution were analyzed with Student t test and expressed as mean and standard deviation. Quantitative variables with a non-normal distribution were analyzed with the Mann-Whitney U test and expressed as median and first and third quartiles. Dichotomous variables were compared with Pearson c2. We considered α≤.05 was statistically significant.
RESULTS
Group 1 consisted of the 71 patients receiving fibrinolysis of 134 admitted with STEAMI (53% thrombolysis) between January 20, 2002 and January 31, 2004. Group 2 consisted of the 80 patients receiving thrombolysis (49.7%) of 161 admitted between February 1, 2004 and February 1, 2006. Baseline characteristics of both groups appear in Table 1.
Myocardial Reperfusion Therapies
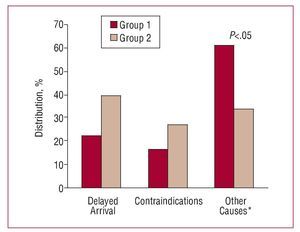
In group 1, 53% of patients received fibrinolysis, whereas 2.2% underwent primary percutaneous transluminal coronary angioplasty (PCTA). In group 2, 49.7% received thrombolysis and 15% underwent primary PCTA. Thus, 55.2% of patients in group 1 were reperfused versus 64.7% of those in group 2 (P<.01). Causes of nonreperfusion appear in Figure 1.
Figure 1. Causes of nonreperfusion. *Other causes: doubts over diagnosis, late diagnosis, absence of pain.
Time to Myocardial Reperfusion
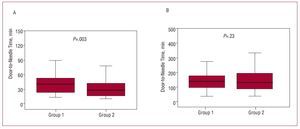
Median (P25-75) door-to-needle time was 40 (23-52) min in group 1 and 27 (15-43) min in group 2 (P=.003). Creating the chest pain service led to a 30% reduction in time to myocardial reperfusion. The distribution of these times appears in Figure 2A. Fibrinolysis was administered in <30 min to 30.6% of patients in group 1 and 56.3% of patients in group 2 (P=.002).
Figure 2. A: box plot of door-to-needle time. B: box plot of myocardial ischemia time.
Reduced door-to-needle time was not associated with reduced ischemia time (from onset of pain to thrombolysis). Median ischemia time (P25-75) was 150(105-195) min in group 1 and 144 (97-212) min in group 2 (P=.23). The distribution of these times appears in Figure 2B. Fibrinolysis was administered at the first 3 h to 64.9% of patients in group 1 and 66.3% in group 2 (P=.86).
In patients undergoing primary PCTA, median (P25-75)door-to-balloon time was 150 (124-170) min in group 1 and 75 (60-122) min in group 2 ( P =.18).Intrahospital Clinical Course and Prognosis at 1-Year Follow-up
Intrahospital clinical course and 1-year prognosis appear in Table 2. Follow-up data is available for 90.1% of patients in group 1 and 93.7% in group 2.
DISCUSSION
Success in treating STEAMI is based on minimizing myocardial ischemia time but recommended objectives3 are difficult to achieve in daily clinical practice (median door-to-needle time recorded in Spain's PRIAMHO II4 registry was 48 min).
Delayed administration of fibrinolytics is due to a wide range of factors such as attending hospital at night or using private transport (ie, not using the ambulance service). Avoiding patients' need to attend ER5 or improving transport, as in the Vienna registry,6 increased the use of reperfusion and cut time intervals. Rapid identification of patients with STEAMI is one objective of chest pain units, although more infrastructure is required.7The new protocol requires no increase in medical personal and minimal additional cost as it is based on prioritizing patients with chest pain. Thus, we achieved a thrombolysis rate of 56% at the first 30 min, which is higher than the 46% reported by McNamara et al8 and similar to that of the GRACE registry, in which median door-to-needle time fell from 35 to 30 min, between 1999 and 2004.9
In patients with STEAMI, prognosis at 1 year depends on many factors—eg, prehospital delay10—which seriously affect ischemia time. Hence, the reduction of door-to-needle time alone seems, a priori, insufficient to achieve long-term improvements in clinical course. Concerted action is necessary and the population needs to be better informed about coronary heart disease and on improvements in the speed of and access to the ambulance service.
However, we found many group 2 patients required revascularization, which can only be explained by the availability of a cardiac catheterization laboratory at our center since June 2003. It is well known that the availability of a technique in a center increases demand for it. If we only analyze patients admitted after June 2003, the difference in revascularization disappears.
In our center, optimizing existing resources by creating a priority chest pain service, has enabled us to reduce door-to-needle time in patients with STEAMI and attend most of these within the clinical practice guideline objective, although this percentage needs increasing further.
ACKNOWLEDGEMENTS
We would like to thank Dr Jorge Morales, Dr Roberto Güerri, and Dr Eduard Terrer for their collaboration in the follow-up of patients.
Correspondence:
Dr. C. García García.
Servicio de Cardiología. Hospital del Mar.
Pg. Marítim, 25-29. 08003 Barcelona. España.
E-mail: CGarciaG@imas.imim.is
Received December 29, 2006.
Accepted for publication December 11, 2007.