Keywords
INTRODUCTION
The presence of factor V Leiden is the most common cause of hereditary thrombophilia.1 The molecular basis for this condition is the substitution of arginine by glutamine in position 506, which results in resistance to the action of activated protein C, such that factor V is inactivated more slowly than usual.2
Clinically, the condition is characterized by the presence of deep venous thrombosis, with or without associated pulmonary embolism, and an increased risk of thrombosis of the cerebral veins. No relationship has been established between the presence of factor V Leiden and arterial thrombosis, but there is an association with antiphospholipid syndrome.3
Our patient presented both these alterations, and they were probably related to the recurrence of acute myocardial infarction.
CASE STUDY
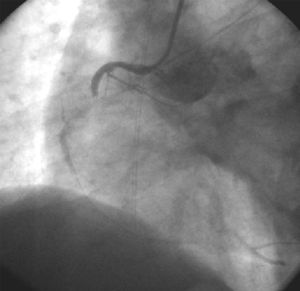
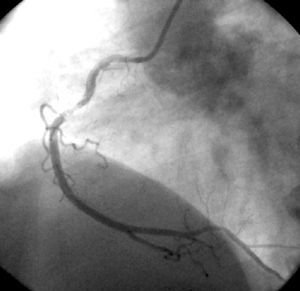
We describe the case of a 54-year-old man with a history of ischemic heart disease represented by an anterior myocardial infarction, who presented with considerable deterioration of left ventricular systolic function (ejection fraction, 30%), hypercholesterolemia, type 2 diabetes, active smoking habit, and human immunodeficiency virus (HIV) infection. The patient was under treatment with didanosine, efavirenz, and tenofovir, and mentioned an allergy to aspirin. On the day of admittance, while at rest, he experienced an episode of oppressive precordial pain that radiated to both arms, with subsequent loss of consciousness. He was taken to his referral hospital in shock. Blood pressure was 80/60 mm Hg and the electrocardiogram showed sinus rhythm at 75 bpm, a lesion wave indicating inferior subepicardial ischemia and another in the right ventricle leads. On the basis of these findings, the patient underwent urgent cardiac catheterization, which showed subtotal occlusion of the mid right coronary artery (Figure 1). The artery was treated with primary angioplasty and stent placement (Figure 2). In addition, significant stenosis was detected in the left anterior descending artery; however, it was not possible to act in this case, since the guidewire could not be further advanced.
Fig. 1. Right coronary angiography on hospital admittance before primary angioplasty, showing a thrombus in the middle third of the artery and subtotal occlusion.
Fig. 2. Right coronary angiography after primary angioplasty with stent placement.
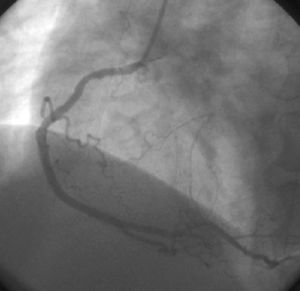
Initially, the patient had a favorable clinical evolution but on the third day after admission, he presented precordial pain and ST-segment elevation in the inferior wall leads. An urgent repeat coronary angiography showed thrombotic occlusion of the stent in the right coronary artery (Figure 3). Balloon PTCA was performed and high doses of intravenous unfractionated heparin were administered. Once flow had been re-established and while the patient was still in the interventional cardiology unit, thrombosis recurred proximal and distal to the stent. Two new stents were implanted in these locations. An urgent coagulation study was requested and factor V Leiden was found, associated with lupus anticoagulant, anticardiolipin antibody and antiphosphatidylserine. In addition, there was a deficit of antithrombin III, probably caused by the high doses of unfractionated heparin used during the percutaneous intervention. To treat this, antithrombin III was administered until normal values were reached. Antiplatelet therapy with clopidogrel was maintained, and anticoagulant treatment, which initially consisted of subcutaneous enoxaparin, was subsequently maintained with oral acenocoumarol.
Fig. 3. Right coronary angiography on the third day after admission for a new acute coronary syndrome with recurrent ST-segment elevation in the inferior aspect, showing thrombotic reocclusion of the right coronary artery in the area of the stent.
The patient remained asymptomatic and progressed favorably. Tests for aspirin allergy were performed, given the importance of confirming this datum. The tests were negative; hence the patient was started on acetylsalicylic acid therapy at a dose of 100 mg/day. He was discharged some days later with the following treatment: acetylsalicylic acid, clopidogrel, acenocoumarol, enalapril, metoprolol, and pravastatin, in addition to his previous antiretroviral therapy.
DISCUSSION
The literature contains few reports of thrombotic complications determining an acute myocardial infarction in the context of systemic diseases other than arteriosclerosis. In the case of factor V Leiden, there is some possibility that thrombosis in a venous territory will occur when it is present.4,5 Nevertheless, no relationship has been established between this alteration and thrombosis in an arterial territory6,7 except in young patients and in association with other clinical risk factors.8
In the patient described, acute myocardial infarction can be explained by the presence of several classic risk factors (diabetes mellitus, hypercholesterolemia, hypertension, and active smoking habit). The patient was treated with stent implantation and the usual medical treatment for these cases (clopidogrel, unfractionated heparin during the procedure, and abciximab), with the exception of aspirin because of a presumed allergy.
Despite appropriate treatment, the patient developed acute stent occlusion. Balloon PTCA was performed and immediately acute intraoperative reocclusion of the stent was observed, a fact that prompted the request for a complete coagulation study to investigate a suspected prothrombotic state.9,10 The coagulation study showed factor V Leiden and lupus anticoagulant, establishing the diagnosis of primary antiphospholipid syndrome. Since the patient had hereditary thrombophilia (factor V Leiden) associated with spontaneous thrombosis in an unusual territory, acenocoumarol therapy was started.11 In addition, antithrombin III deficit was detected, probably due to the use of high doses of heparin; the deficit was corrected with administration of antithrombin III. Tests to investigate a presumed aspirin allergy mentioned by the patient during the anamnesis were negative; hence, treatment with acetylsalicylic acid at a dose of 100 mg/day was initiated.
The existence of primary antiphospholipid syndrome does not vary the therapeutic approach, but it does provide a new perspective to explain the patients' clinical picture. The coexistence of factor V Leiden and antiphospholipid syndrome is related to a higher probability of developing acute myocardial infarction and a higher tendency to present thrombosis in an arterial territory,3 whereas antiphospholipid syndrome alone only favors the development of acute myocardial infarction.12 It should also be mentioned that the patient was receiving antiretroviral treatment for HIV infection, and a recent report has related this to a higher probability of developing acute myocardial infarction.13
This case shows that the coexistence of factor V Leiden, primary antiphospholipid syndrome and HIV infection under antiretroviral treatment, in addition to the classic risk factors for coronary disease, was related to the development of acute myocardial infarction and recurrent in-stent thrombosis.
Correspondence: Dr. I. Cruz González.
Servicio de Cardiología. Hospital Universitario de Salamanca.
Paseo San Vicente, 58-182. 37007 Salamanca. España.
E-mail: ignacio_cruz_gonzalez@hotmail.com