Bicuspid aortic valve (BAV) is a congenital defect consisting of the anatomical fusion of 2 aortic valve leaflets. This defect is associated with a high prevalence of aortic dilation, whose hemodynamic or genetic origins are the subject of debate. Raphe, the conjoined area of 2 adjacent defective leaflets, is common in BAV and has recently attracted the interest of research. Indeed, in a large multicenter study, the presence of raphe was associated with increased aortic surgery rates.1 Raphe has also been related to a higher prevalence of significant aortic stenosis1,2 and regurgitation.1 Although aortic blood flow abnormalities have been associated with aortic extracellular matrix dysregulation and fiber degeneration3 and dilation4,5 in bicuspid aortopathy, the influence of the presence of raphe in ascending aorta blood flow has not yet been established. The aim of the present research letter was to ascertain whether BAV with raphe is associated with differences in flow pattern or aortic stiffness vs BAV without raphe in the absence of significant aortic valve disease.
Eighty-seven adults with BAV with a single fusion covering> 50% of the leaflet and no significant aortic valve disease (aortic regurgitation ≤ 10%, aortic velocity<2 m/s on cardiac magnetic resonance [CMR]) referred for CMR study were consecutively and prospectively recruited from our Aortic Unit. Inclusion criteria were the absence of cardiovascular disease, connective tissue disorders, congenital heart disease, and contraindication for CMR. Because the presence of a single fusion was assessed by CMR, we cannot exclude the existence of other minor fusions potentially missed by this imaging technique. The study was approved by the local ethics committee and informed consent was obtained from all participants. The CMR protocol included several bSSFP cine images to assess BAV morphology and aortic diameter and a 4D phase-contrast CMR (4D flow magnetic resonance imaging) acquisition with retrospective electrocardiogram-gating during free-breathing to quantify aortic flow pattern and regional aortic stiffness. For 4D flow magnetic resonance imaging, a phase-contrast vastly undersampled isotropic projection sequence with an isotropic spatial resolution of 2.5 mm, a temporal resolution of 26.9±2.4ms and a velocity encoding of 200 cm/s was used as previously described.4 Average acquisition time was 10minutes and endovenous contrast was not given.
Aortic 3D geometric models were semiautomatically reconstructed from 3D phase-contrast magnetic resonance angiography and used to mask 4D flow data. Common descriptors of aortic blood flow were computed at 8 planes in the ascending aorta, equidistantly distributed between the sinotubular junction and the brachiocephalic trunk. Flow normalized displacement, a marker of flow asymmetry, in-plane rotational flow describing flow rotational behavior and systolic flow reversal ratio, which quantifies vortex intensity, were computed as previously described.4 Moreover, maps of axial and circumferential wall shear stress at systolic peak, a variable directly related to aortic wall disruption,3 and ascending and descending aorta pulse wave velocity, which quantifies regional stiffness, were obtained.4,6 Using SPSS 21 software (IBM, Chicago, Illinois), continuous variables were compared using the Student t-test if normally distributed and the Mann-Whitney U test otherwise, while the chi-square test was used for categorical variables. A 2-tailed P value <.05 was considered statistically significant.
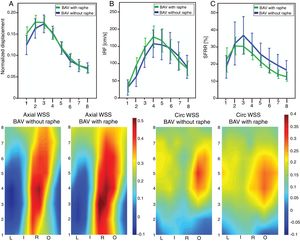
Most BAV patients had raphe (54/87, 62%). BAV patients with and without raphe did not differ in age (47±13 vs 51±15 years, respectively, P=.436), sex (63% vs 52% male, P=.293), body surface area (1.83±0.19 vs 1.78±0.23 m2, P=.411), ejection fraction (61±8 vs 60±7%, P=.436), maximum ascending aorta (40.2±7.6 vs 41.0±7.3 mm, P=.713), and root (35.9±4.5 vs 35.9±4.8 mm, P=.823) diameters, or in the prevalence of hypertension (75% vs 64%, P=.262) and right and left cusp fusion phenotype (81% vs 70%, P=.256). No statistically significant differences were found in ascending (4.2±2.6 vs 3.3±1.1, P=.170) and descending (11.2±5.0 vs 10.7±4.8, P=.765) pulse wave velocity when BAV patients with and without raphe were compared. Furthermore, no statistically significant differences were found when BAV patients with and without raphe were compared in any analysis planes (planes 1 to 8) regarding normalized displacement, in-plane rotational flow and the amount of systolic flow reversal (Figure 1A, B and C, respectively). Moreover, no statistically significant differences were found in axial and circumferential wall shear stress maps between these 2 groups (Figure 1, bottom).
Flow descriptors. A: normalized displacement. B: in-plane rotational flow (IRF). C: systolic flow reversal ratio (SFRR) at 8 planes between the sinotubolar junction (plane 1) and the brachiocephalic trunk (plane 8) in bicuspid aortic valve (BAV) patients with (green) and without (blue) raphe. Bars show the 5th and 95th percentiles. Bottom: axial (left) and circumferential (circ, right) wall shear stress (WSS, [N/m2]) in bicuspid aortic valve patients with and without raphe. I, inner; L, left; O, outer; R, right.
In BAV patients with a single fusion covering> 50% of the leaflet and no significant aortic valve disease as evaluated by cine CMR, the presence of raphe was not related to the degree of dilation, ascending aorta flow patterns or local aortic stiffness. Consequently, this aortic valve characteristic should not imply different clinical management from that established by its valvular morphotype and the severity of both valvular heart disease and aortic dilation.
FUNDINGThis study was funded by Instituto de Salud Carlos III [grant number PI17/00381], La Marató de TV3 [grant number 20151330), Ministerio de Economía y Competitividad through Retos-Colaboración 2016 [grant number RTC-2016-5152-1], Beca Philips de la Societat Catalana de Cardiologia 2017 and CIBERCV.
A. Guala received funding from the European Union Seventh Framework Programme FP7/People [grant agreement 267128].
We are grateful to Augusto Sao Avilés for support during statistical analysis and Christine O’Hara for English revisions.

![Flow descriptors. A: normalized displacement. B: in-plane rotational flow (IRF). C: systolic flow reversal ratio (SFRR) at 8 planes between the sinotubolar junction (plane 1) and the brachiocephalic trunk (plane 8) in bicuspid aortic valve (BAV) patients with (green) and without (blue) raphe. Bars show the 5th and 95th percentiles. Bottom: axial (left) and circumferential (circ, right) wall shear stress (WSS, [N/m2]) in bicuspid aortic valve patients with and without raphe. I, inner; L, left; O, outer; R, right. Flow descriptors. A: normalized displacement. B: in-plane rotational flow (IRF). C: systolic flow reversal ratio (SFRR) at 8 planes between the sinotubolar junction (plane 1) and the brachiocephalic trunk (plane 8) in bicuspid aortic valve (BAV) patients with (green) and without (blue) raphe. Bars show the 5th and 95th percentiles. Bottom: axial (left) and circumferential (circ, right) wall shear stress (WSS, [N/m2]) in bicuspid aortic valve patients with and without raphe. I, inner; L, left; O, outer; R, right.](https://static.elsevier.es/multimedia/18855857/0000007300000001/v1_201912301211/S1885585719301847/v1_201912301211/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6IkRYTGh1WUwyZWNTWXhONlJOWFFWZGc9PSIsInZhbHVlIjoiajNpSHhONFV1emZmVFhETXppcm0waldiVzRlajc1em9WaTkyUXM2aWY1dz0iLCJtYWMiOiJlMjQzMjA0ZjVjMDYxMTUzNWM1Y2E0NTkyY2UwMGJkYzAzNmZlNTFjOWUyYjcwNzMxNzYyYzRkOTA4NGZiOTE0IiwidGFnIjoiIn0=)