Keywords
It is well-known that pulmonary hypertension can complicate infection by the human immunodeficiency virus (HIV). The incidence of primary pulmonary hypertension in HIV positive patients is unknown, but could be higher than 0.5%, in comparison with an 0.02% incidence in the general population. Since 1987, 131 cases of pulmonary hypertension associated with HIV infection have been published.1 A total of 76 patients presented with primary pulmonary hypertension.2 Among the 76 cases, 61.8% were men, while there was a slight predominance of women among the cases of primary pulmonary hypertension not associated with HIV infection (approximately 1.7 to 1).
The clinical and histopathological findings of primary pulmonary hypertension in HIV infection do not differ from those of classic primary pulmonary hypertension. The diagnosis should be highly suspected, and a careful evaluation to should be performed to exclude secondary pulmonary hypertension in patients infected with HIV. Some risk factors for the development of pulmonary hypertension associated with HIV infection are known, including the use of intravenous (IV) drugs, chronic liver disease, and coagulation changes with embolic phenomena.
The pathogenesis of primary pulmonary hypertension in patients positive for HIV is unknown. It is speculated that the virus may act via the liberation of mediators.
We describe 4 cases of primary pulmonary hypertension in patients with HIV infection who were admitted to our center during the last 3 years.
CLINICAL CASES
Case 1
A 30-year-old man with a history of smoking and occasional use of marijuana. The patient was admitted for chest pain and effort dyspnea for 1 week. Upon admission he was in good general health, without cyanosis. Cardiac auscultation revealed a II/VI systolic murmur in the tricuspid focus, a rougher murmur in the aortic focus, a second divided noise with an increase in the pulmonary component, and a fourth noise. Pulmonary auscultation was normal.
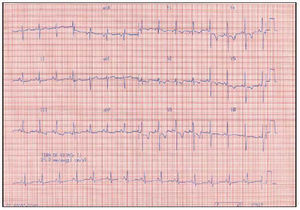
Electrocardiogram revealed the existence of a sinus rhythm, right atrial enlargement, and signs of ventricular hypertrophy (Figure 1).
Fig. 1. 12-lead electrocardiogram of a patient with pulmonary hypertension.
Chest x-ray showed enlargement of the right cardiac cavities, without protrusion of the pulmonary artery trunk or the principal pulmonary arteries. The cardiac silhouette was ovoid in shape, with a narrow pedicle. There were no evident signs of pulmonary hypertension. Analyitic tests and hemogram were normal.
Transthoracic echocardiography revealed dilatation of the right atrium, protrusion of the intra-atrial septum toward the left atrium, and dilatation and hypertrophy of the right ventricle with a telediastolic diameter of 38 mm and 8 mm free wall. Moderate tricuspid insufficiency was seen. The systolic arterial pressure was 86 mm Hg. The left valves were normal, as was ventricular function.
Cardiac catheterization was performed, and obstructive lesions were seen in the coronary artery tree. After 7 months, the patient was readmitted with the same symptoms. On transthoracic echocardiogram a significant dilatation of the right ventricle was seen (DTDVD, 42 mm), as was a normal size left ventricle. The dilatation of the right atrium was 75 mm. Tricuspid insufficiency was seen that allowed an estimation of the systolic pulmonary pressure of 86 mm Hg. A slight pericardial leak could be seen. Pulmonary perfusion gammography did not reveal segment defects suggestive of pulmonary thromboembolism. The patient died of cardiac arrest 3 days after admission.
Autopsy revealed violet-colored lungs, without crepitation, congested, and weighing 650 g. The heart weighed 480 g, with right cavity enlargement. The pulmonary artery had atheromatous deposits that extended up to the principal branches. The liver and spleen had a congestive appearance and were accompanied by scant ascitic liquid.
Among the microscopic pulmonary findings, the most significant was the presence of plexiform lesions, with multiple vascular canals and fibrosis of the pulmonary artery wall. There was no arterial thrombosis.
During the autopsy, HIV and hepatitis blood work was performed, and was positive for HHIV and hepatitis C.
Case 2
38-year-old man, with a history of HIV infection (diagnosed in 1997), chronic liver disease by hepatitis C and hepatitis B and delta, with hepatic cirrhosis. In April of 1997, he was admitted with dyspnea, general malaise, and palpitations. On physical examination he was in a generally good state of health, without fever. Cardiac auscultation revealed rhythmic tones and a III/IV systolic murmur in the tricuspid focus. Pulmonary auscultation did not reveal pathological findings.
Electrocardiogram revealed a sinus rhythm, complete block of the right branch and signs of right ventricular hypertrophy. Chest x-ray showed cardiomegaly of the right cavities. Transthoracic echocardiography showed dilatation of the right cavities (DTDVD, 50 mm). The existence of hypertrophy of the right ventricle was seen. Moderate tricuspid insufficiency was seen, allowing an estimation of the systolic pulmonary pressure at 73 mm Hg. Abdominal echocardiography revealed uniform hepatosplenomegaly and a minimum quantity of perivisceral ascitic liquid. Right cardiac catheterization was performed, revealing pre-capillary pulmonary hypertension, with a median pulmonary artery pressure of 45 mm Hg at rest and vascular pulmonary resistance of 609 dyne/cm².
Treatment with calcium antagonists was begun, which the patient discontinued. He returned some months later for a high digestive hemorrhage related to esophageal varices, and died secondary to liver failure.
Case 3
69-year-old man, diagnosed with HIV infection, who on admission presented with cerebral toxoplasmosis. He went to the hospital because of a 4-month history of effort dyspnea. On physical examination, he was in generally good health, without cyanosis. Cardiopulmonary auscultation was normal. Analytical data only revealed a normocytic-normochromic anemia. Biochemical parameters did not indicate significant changes.
Chest x-ray revealed overall cardiomegaly, bilateral interstitial infiltrate, and vascular redistribution toward the pulmonary vertices.
Echocardiography revealed dilatation of the right cavities with 45 mm DTDVD. Tricuspid insufficiency was noted that permitted calculation of a systolic pulmonary pressure of 80 mm Hg (Figure 2). Pulmonary perfusion gammography was performed and there was no evidence of thromboembolism. Spirometry revealed normal airway fluid values.
Fig. 2. Transthoracic echocardiogram of a patient with pulmonary hypertension. Parasternal axis plane cut in which dilatation of the right ventricle can be seen.
The patient was discharged with the diagnosis of pulmonary hypertension associated with HIV infection, and nifedipine treatment was initiated. In control echocardiography (at 2 months), the systolic pulmonary pressure had decreased to 50 mm Hg.
Case 4
31-year-old woman, a smoker, with HIV infection. She presented with negative blood work for hepatitis B and C. She was admitted for a dry cough and dyspnea with moderate effort, without other symptomatology.
Chest x-ray showed an increase in the outlet cone of the pulmonary artery. Transthoracic echocardiography revealed dilatation of the right cavities. A slight tricuspid pulmonary insufficiency was observed. The systolic pulmonary pressure was calculated to be 75 mm Hg.
Among the laboratory data a slight polyclonal hypergammaglobulinemia stood out. Spirometry showed normal values.
Pulmonary perfusion gammography revealed the absence of segment defects suggestive of pulmonary thromboembolism.
The patient was discharged with anti-retroviral treatment. At 2-year followup she had dyspnea with minimum effort.
Table 1 shows the antecedents, hemodynamic data, and treatment of the cases described.
DISCUSSION
The first case of pulmonary hypertension associated with HIV infection was described in 1987 by Kim and Factor,3 in a hemophiliac patient who also had membrane proliferative glomerulonefritis. Later, Goldsmith described 5 patients with HIV infection, hemophilia, and pulmonary hypertension.4 At a later date, cases were published of patients who did not have hemophilia who had pulmonary hypertension, and consideration was given as to whether the latter was related to HIV infection.
The incidence of primary pulmonary hypertension in patients with positive HIV infection is not well known, but has been described as being greater than that in the general population. Among the 76 cases described, median age was 33 years. The majority the cases were men (61.8%). In reviewing the published cases, the risk factor for HIV infection was intravenous drug use in 50% of cases, homosexual contact in 19.7%, hemophilia in 13.2%, heterosexual contact in 9.2%, blood transfusion in 3.9% and bisexual contact in 1.3%.2
The pathogenesis of primary pulmonary hypertension in HIV positive patients is unknown. It is speculated that the virus could act via the liberation of mediators. Cytokines, particularly endothelin 1, have been implicated in the pathogenesis of this illness.5 Genetic predisposition has a role in the development of pulmonary hypertension in these patients, given that it is not related to the level of immunodepression or the recount of CD4 cells, and only a minority of the patients who were HIV positive developed pulmonary hypertension. A greater prevalence of HLA-DR6 and HLADR52 has been described in patients infected with the HIV virus with pulmonary hypertension.6
The diagnosis of pulmonary hypertension in HIV positive patients should be highly suspected clinically. The principal symptom is dyspnea. Other symptoms are related to right cardiac insufficiency, syncope, chest pain, and non-productive cough. The prospective study carried out by Petitpretz7 compared a group of 20 HIV positive patients who presented with pulmonary hypertension with 93 patients who were not HIV infected but had primary pulmonary hypertension. The 2 groups differed in age (32 vs 42 years, respectively), functional class (NYHA class III or IV: 50% vs 75%, respectively) and the value of pulmonary hypertension (mean pulmonary artery pressure 50±11 vs 62#+15 mm Hg, respectively). The prognosis for patients with pulmonary hypertension associated with HIV infection is worse than that of HIV positive patients without pulmonary hypertension. The cause of death in these patients is attributable to pulmonary hypertension in 81% of cases, with right cardiac insufficiency in 76% of the cases and sudden death in 20%. The death of the patient in case 1 was attributed to pulmonary hypertension. The symptoms of pulmonary hypertension are not specific in HIV positive patients. Physical examination may reveal signs of pulmonary hypertension (increase in the pulmonary component of the second noise, fourth cardiac noise, tricuspid insufficiency, etc.) or findings of right cardiac insufficiency (edema, ascitis, and hepatomegaly). Chest x-ray is abnormal in 84% of cases, with cardiomegaly and prominence of the pulmonary artery trunk being frequent findings. Electrocardiogram shows the changes in 89% of cases, typical findings being deviation of the axis toward the right and right ventricular hypertrophy. Echocardiography is useful for eliminating the diagnosis of myocardial dysfunction, valve disease, or pericardial disease. Pulmonary ventilation/perfusion gammography is essential for excluding pulmonary thromboembolism. When the result is not conclusive, pulmonary angiography should be considered. Pulmonary function studies tend to be normal or to reveal a slight restrictive defect, with a decrease in carbon monoxide diffusion capacity. Obstruction of peripheral airways has been described in cases of pulmonary hypertension. Hyperinsuflation without obstruction of the airways has also been described in a patient with pulmonary hypertension who was HIV positive. Cardiac catheterization is required to confirm the diagnosis of pulmonary hypertension and determine therapy. Pulmonary biopsy is not considered essential for establishing the diagnosis, although it may be useful in individual cases, especially when other diseases associated with pulmonary hypertension are present. Pulmonary hypertension secondary to the use of IV drugs cannot be excluded without a pulmonary biopsy.
Among the cases described, 1 patient presented with cirrhosis of the liver. Several studies have described the association between pulmonary hypertension and portal hypertension, as well as the risk of developing pulmonary hypertension increasing with the duration of portal hypertension.8
The therapy of choice for pulmonary hypertension associated with HIV infection is unknown. Treatment with oral anticoagulants and vasodilators is indicated, and has been related to the survival of patients with classic pulmonary hypertension.9 Clinical, histopathological, and hemodynamic similarities between hypertension associated with HUIV infection and classic pulmonary hypertension suggests that HIV positive patients would benefit, if there is response to treatment, from chronic vasodilator therapy. The response to vasodilators is unpredictable, even unfavorable at times, so that an acute test must be performed prior to initiating treatment.9 One of our patients received calcium antagonist treatment and experienced clinical improvement and an improvement in pulmonary systolic pressure during the followup period.
Treatment with oral anticoagulants has been utilized for pulmonary hypertension related to HIV infection, although its efficacy is uncertain. Anti-retroviral therapy is frequently used in the treatment of pulmonary hypertension associated with HIV. Some authors recommend initiating anti-retroviral treatment in all HIV positive patients with primary pulmonary hypertension, regardless of the CD4 recount and the viral load. One study of HIV positive patients treated with anti-retroviral agents showed a decrease in the right atrioventricular pressure gradient vs a group of HIV patients who were not treated.10 Recently, a study described a lesser incidence of cardiac involvement, including pulmonary hypertension, in HIV positive patients treated with highly active anti-retroviral therapy.11 Epoprostenol (prostacycline) and calcium channel blocker therapy has been shown to have variable efficacy in different published series. It has also recently been found that acute and long-term treatment with epoprostenol may improve the functional and hemodynamic status of patients with pulmonary hypertension associated with HIV infection.12
It must be pointed out that, from a clinical perspective, the search for non-infectious causes of dyspnea in HIV infected patients is important. The appearance of unexplained cardiopulmonary symptoms in HIV positive patients must suggest the presence of pulmonary hypertension. The development and progression of pulmonary hypertension is not related to the stage of HIV infection.
Correspondence: Dra. M.A. Martínez Torres.
Servicio de Cardiología. Hospital Universitario Virgen de Valme.
Ctra. Cádiz, s/n. Sevilla. Spain.
E-mail: angiefr@teleline.es