Keywords
INTRODUCTION
Primary cardiac tumors (PCTs) are rare. Around 25% of these tumors are malignant1 and 90%-95% of malignant tumors are sarcomas.2 They may remain clinically silent for a long time or cause a range of cardiac and systemic symptoms that mimic other diseases.3-6
The preferred initial method for detecting cardiac tumors is echocardiography, but a complete assessment of the heart and surrounding tissue may sometimes be difficult with this technique. Magnetic resonance (MR) imaging and computed tomography (CT) can provide precise information on the extent of involvement of the tumor.4,7-9 Moreover, these techniques allow simultaneous evaluation of cardiac structures and surrounding tissue and, in certain instances, a guided biopsy is possible.
We report the use of different imaging techniques to determine the clinical and morphologic characteristics of the hearts of 3 patients who underwent interventions for cardiac angiosarcomas.
CASE STUDY
Between 1995 and 2002, 3200 patients underwent open-heart surgery. Three of these (0.0009%) were patients who had cardiac masses diagnosed by imaging techniques. Diagnosis of cardiac angiosarcoma was confirmed by biopsy in all 3 patients. These patients are discussed below.
Case 1
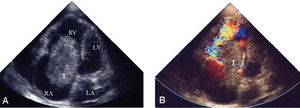
The patient was a 19-year-old man with functional grade 3 dyspnea, skin and mucous membrane pallor, and a grade 3/6 systolic murmur audible in the fourth and fifth right intercostal spaces. The echocardiogram showed a solid mass of variable density measuring 6x4.5 cm in the right atrium (RA) that had invaded the atrial septum (Figure 1A). In the enhanced T1-weighted MR images (Figure 1B), a proliferative mass that had invaded almost the entire right ventricle (RV) was evidenced, displacing the atrial septum to the left. Moderate left pleural effusion and retrocardiac atelectasis were also found. No signs of metastasis to abdominal organs were observed with abdominal MR imaging or echography. Surgical intervention confirmed a large RA tumor that had invaded the RV and the septal region of the tricuspid valve. The tumor was resected, the tricuspid valve reinserted and a venous bypass to the right coronary artery performed. The biopsy confirmed diagnosis of primary angiosarcoma. After 6 months, the patient presented with refractory heart failure and died.
Figure 1. A: transthoracic echocardiogram in subcostal 4-chamber projection showing a tumor (T) that occupies almost the entire right atrium and part of the right ventricle (RV). B: spin-echo enhanced T1 axial plane image of invasion of the right atrium by the tumor. LA indicates left atrium; LV, left ventricle.
Case 2
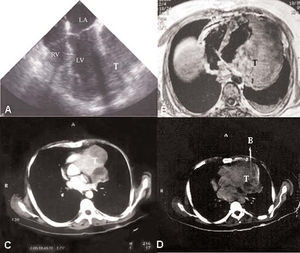
A 32-year-old woman with dyspnea at rest and of emaciated appearance was experiencing tachycardia on admission to hospital. A grade 3/6 diastolic murmur--maximal in the tricuspid region--was audible and she presented jugular engorgement and leg edema. The echocardiogram revealed a large solid RA mass measuring 6x4 cm (Figure 2A and B) with regions of low signal intensity. The mass had a base of attachment to the atrial septum and invaded the tricuspid valve causing severe flow obstruction with maximum tricuspid gradient of 15 mm Hg. The patient went into cardiogenic shock and required emergency heart surgery. In the RA, a large tumor measuring 7x4 cm was found that invaded the RV through the tricuspid valve. The base of attachment extended towards the RA free wall and towards the opening of the inferior vena cava. No hepatic metastasis was observed in abdominal CT or echography. The tumor was resected and the atrium reconstructed with a bovine pericardial patch. Biopsy confirmed the diagnosis of angiosarcoma. After 1 year of follow up, the patient presented with progressive dyspnea and refractory congestive heart failure and died.
Figure 2. A: Transthoracic echocardiogram in 4-chamber apical projection, showing an oval tumor (T) in the right atrium (RA) that has invaded the right ventricle (RV). A central region of lower signal intensity suggests a region of necrosis. B: Turbulent flow in color Doppler imaging due to obstruction of the tricuspid valve. LA indicates left atrium; LV, left ventricle.
Case 3
A 50-year old man with atypical pain in the left side of the chest, asthenia, and adynamia presented with weight-loss and tachycardia at rest. In the echocardiogram, a solid mass could be seen measuring 8x11 cm with transparent regions in the lower, lateral and apical walls of the LV (Figure 3A). The enhanced T1-weighted MR images (Figure 3B) showed a large tumor of 14x11 cm, with variable T2-weighted signal strength. Lytic lesion of the costal arch and mild pleural effusion were also observed. Chest CT (Figure 3C and D) defined the edges of the tumor and allowed a guided biopsy without complications. The biopsy confirmed diagnosis of angiosarcoma. Abdominal CT and echography revealed no metastasis to abdominal organs. The tumor could not be resected during surgery because the extent and anatomical involvement were too great. The patient died 10 days after the operation.
Figure 3. A: transesophageal echocardiogram showing a solid tumor (T) with a heterogeneous structure attached to the lateral wall of the left ventricle (LV). B: spin-echo enhanced T1 axial plane image showing a large solid tumor with involvement of the LV lateral wall, and with variable signal intensity indicative of tumor necrosis. C: helicoidal computed tomography with contrast showing section of the aortic root. The left heart outline is deformed by a multi-lobed mass with regions of variable intensity. D: computed tomography with biopsy needle (B). LA indicates left atrium; RV, right ventricle.
DISCUSSION
Malignant PCTs may present with any cardiac symptom,1,3,4,10 but heart failure and systemic embolism are the most common ones initially.5,11 Two of our patients showed signs of heart failure and one had atypical chest pain.
In this series of patients, the initial diagnostic technique was echocardiography, although MR imaging provided greatest additional information. Thus, the extent of the tumor could be precisely defined,4,12 so facilitating the decision on how to proceed (the approach used and whether to resect the tumor).8,13 Computed tomography allowed diagnosis of the third patient by guided biopsy prior to surgery.
Echocardiography has the advantage of being a cheap and readily available technique that can be done at the patient's bedside with no contraindications. However, it is sometimes difficult to define what structures have been invaded by the tumor. A benign tumor may also be falsely diagnosed, as in the second of our patients, because the echocardiographic images resemble those of atrial myxoma, something that has been reported occasionally in the medical literature.14
Magnetic resonance imaging has the advantage of providing better image quality and a more precise characterization of the tumor (density, extent, and invaded cardiac structures). It also allows assessment of involvement of other neighboring structures at the same time. The most significant characteristics of malignancy in the MR images are the size of the base of attachment of the tumor to the myocardial wall, the tumor size, compression of the cardiac chambers or the great vessels, pericardial or extracardial involvement and signs of tumor necrosis.15 Although there are no pathognomonic signs, MR images show the angiosarcoma as a tumor mass, usually with no spindle structures, and with weak areas of signal intensity in the enhanced T1-weighted scan, attributed to regions of tumor necrosis.9,16 In rhabdomyosarcomas, the intermediate signal intensity in the enhanced T1-weighted scan is similar to that found in adjacent myocardium.17 Fibromas appear heterogeneous with the same signal intensity in the enhanced T1-weighted scan16 and the malignant nature of the tumor can be discerned with enhanced T1-weighted images.
Computed tomography is better able to define calcification, the study time is shorter, and the technique is useful when MR imaging is contraindicated. Guided transthoracic biopsies are possible with this technique in some patients.18
CONCLUSIONS
We present 3 patients with angiosarcoma in whom echocardiography provided preliminary diagnosis. Magnetic resonance best established the extent of the tumor and CT allowed diagnosis by means of biopsy in one patient. Surgery confirmed the definitive diagnosis and the short-term outcome was death in all 3 patients.
Correspondence: Dr. G. Romero-Farina.
Servicio de Cardiología. Hospital Universitari Vall d'Hebron.
Pg. Vall d'Hebron, 119-129. 08035 Barcelona. España.
E-mail: gromero@vhebron.net