Keywords
INTRODUCTION
Ventricular septal defect (VSD) is the most common congenital heart disease. Spontaneous closure of small defects occurs before the age of three in approximately 45% of patients. Nevertheless, in patients with larger defects, the need for corrective treatment is considered. Surgical closure has yielded excellent results.1,2 Percutaneous closure is a recent technique that offers a less aggressive and more comfortable mechanical alternative. The aim of this article is to analyze our initial experience in 15 patients with VSD, in whom percutaneous closure was attempted.
METHODS
Patients
Between February 2004 and February 2005, percutaneous VSD closure was performed in 15 patients. The defect was located in the muscular septum in 4 patients (26%) and in the perimembranous portion in 11 patients (73%) (3 cases with an associated septal aneurysm). Seven patients were lactating infants (mean age 12±2.4 months) with clinical symptoms of dyspnea, delays in weight gain (mean weight, 7.9±1.9 kg) and sweating when feeding. Among the 8 adults, 4 presented repeated respiratory infections, one had an ischemic cerebral event, and 3 were asymptomatic. One infant had VSD and associated pulmonary stenosis, which had been successfully dilated in a prior procedure. One adult with subaortic VSD had an associated patent foramen ovale (PFO) with prior symptoms of a transient ischemic attack due to paradoxical embolism. During the same procedure, each defect was closed with an Amplatz device.
Diagnostic Catheterization
The procedure was undertaken under general anesthesia and transesophageal monitoring. Previously, a right and left hemodynamic study was performed. In addition, left ventriculography was done in 2 views: LAO 30°-cranial 40° and LAO 70°-cranial 20°. Subsequently, the defect was measured by angiography and echocardiography.
Therapeutic Phase
The diameter of the devices selected was between 2 mm and 3 mm greater than the diameter of the defect as measured by transesophageal echocardiography. An arteriovenous shunt was established with the exchange guidewire. The approach used to create the shunt varied according to the location of the defect:
Muscular VSD (n=4): a Terumo guidewire was passed from the left to the right ventricle through the VSD and advanced to the pulmonary artery. A mammary catheter was advanced over the guidewire to this vessel, the Terumo guidewire was withdrawn, and a long (260 cm), 0.35 inch exchange guidewire was inserted. The end of this guidewire was snared with a loop inserted in the jugular vein. Subsequently the Amplatz muscular VSD occluder sheath was introduced in the jugular and advanced to the left ventricle, where the shunt was eliminated to insert the prosthesis.
Perimembranous VSD (n=11): the same process as described was performed, with the exception that the guidewire was snared and the sheath inserted through a femoral vein route. In both cases, the sheath was inserted through a venous access to reach the left ventricle. Once the device (Amplatz membranous VSD occluder) had been connected, proper location was confirmed by angiography and echocardiography before deployment. In patients with a subaortic VSD, aortography was also performed before releasing the device to ensure that the aortic sigmoid arteries had not been compromised.
Following the procedure, all patients were treated with subcutaneous dalteparin for 1 month and aspirin for 6 months, as well as antibiotic prophylaxis to prevent endocarditis. Patients were closely monitored by frequent telephone contacts, and clinical follow-up visits were performed at 3, 6, and 12 months.
RESULTS
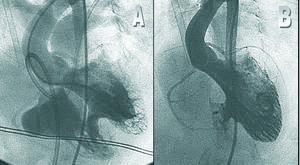
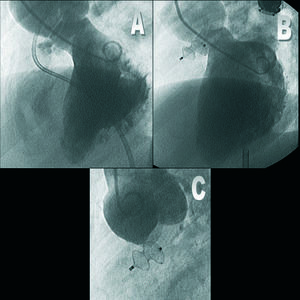
The main baseline and procedure-related data are shown in Table 1. Immediate results are summarized in Table 2. Proper implantation of the device was achieved in 12 of the 15 patients (80%). In the 3 remaining patients, the device could not be stabilized; hence, it was removed as a safety measure without incidents. Complete closure of the defect was observed in 11 of the 12 patients with a satisfactory implant (Figures 1 and 2). In the majority (8/12), immediate, complete closure was documented on angiography. Aortic valve function was not affected in any of the patients with subaortic VSD receiving an implant (Figure 2). Pulmonary arterial pressure decreased significantly in the patients with elevated values. Following closure, the flow ratio approached 1 in all patients.
Figure 1. A: left ventriculography in a LAO 30°-cranial 40° view showing a 7 mm muscular VSD. B: the same view following closure of the defect with a 10 mm Amplatz device, which is correctly positioned and shows no residual shunting.
Figure 2. Angiographic study of a 20-year-old patient with a subaortic VSD. A: left ventriculography in a LAO 70°-cranial 20° view showing a subaortic VSD with an aneurysm. B: the same view following closure, with a favorable posterior results. C: Posterior aortography, showing no aortic regurgitation. Note proper positioning of the occluder (radio-opaque marker in a position opposite to the sigmoids, as well as the absence of aortic sigmoid compromise.
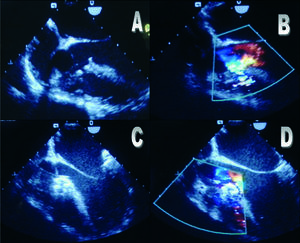
There were no major complications or embolism of the device. Two patients experienced some type of rhythm or conduction abnormality (nodal rhythm and left bundle branch block) following implantation, which were transient. The echocardiographic images of a subaortic VSD in which immediate successful closure was achieved are shown in Figure 3.
Figure 3. Echocardiographic study in the same patient (Figure 2). A and B correspond to the 2-D study and the color Doppler study, in which the VSD and a small subaortic membrane are seen. Following the procedure (C and D) the device is seen to be correctly positioned, with no residual shunting according to the color, as well as disappearance of the membrane.
Following closure, the clinical course was favorable in all patients, particularly the group of infants with heart failure, who showed a considerable clinical improvement and weight gain. The mean weight of the infants treated increased from 7.5±2.5 to 13.4±7 kg. After a mean follow-up of 9.2±3.6 months there were no embolic complications or cases of endocarditis, and all the patients treated were asymptomatic at the time of writing.
In the latest transthoracic Doppler echocardiography study, all the patients showed complete closure. At medium-term, aortic valve function was not compromised in any of the patients with a subaortic implant.
DISCUSSION
Percutaneous closure of a ventricular septal defect is a recent technique that seems to minimize the risks involved in treating this entity and provides excellent results. In recent years the percutaneous technique has undergone substantial development and various series of patients with satisfactory percutaneous closure have been reported.3-16 Correction of the defect is necessary in symptomatic patients and percutaneous treatment has been shown to be a viable alternative whenever possible. In asymptomatic patients over three years of age without hemodynamic repercussions in whom spontaneous closure is an exception, there have been discrepancies about whether to apply surgical treatment because of the associated risks. Nevertheless, some authors have indicated that morbidity and mortality is higher in patients who do not undergo correction.17,18 This group of patients can be considered candidates for percutaneous closure. The appearance of immediate or delayed arrhythmias, such as conduction abnormalities or atrioventricular block, is a potential complication of percutaneous closure, as well as surgical closure (in some surgical series, a more than 40% incidence of right bundle branch block following right ventriculotomy, which is usually transient).19 Although larger series are required, the incidence of these complications seems to be lower following percutaneous closure.
Various types of closure devices have been used previously for this condition.3,5,6 Nevertheless, their use has been gradually discontinued since the introduction of the Amplatz device, which has shown important advantages with respect to the earlier ones.9-18
In our initial series, closure was achieved in 80% of the cases without major complications and with a favorable evolution at follow-up. These findings are similar to the reported results from other series. Nevertheless, the experience is still limited and the follow-up in months is too short to draw definitive conclusions. The initial results are promising and indicate that in the near future, many of these defects can be treated using a percutaneous approach.
Correspondence:
Dr. J. Suárez de Lezo.
AININCAR, Apto. 2.031.
14080 Córdoba. España.
E-mail: grupo_corpal@arrakis.es
Received May 12, 2005.
Accepted for publication November 3, 2005.