To the Editor:
The classically accepted risk factors for atherothrombosis do not explain all cases of stroke and acute coronary syndromes.1 Various hereditary (among others, factor V Leiden mutation, G20210A variant of prothrombin, and antithrombin and protein C or S deficiencies) and acquired (antiphospholipid syndrome, use of estrogens, etc) hematologic disorders--the so-called thrombophilias--can favor those conditions by provoking a state of hypercoagulability.2
We present a case of recurrent arterial and venous thrombosis associated with 2 prothrombotic conditions: protein C deficiency and mutation C677T in methylenetetrahydrofolate reductase (MTHFR). The involvement of these genetic polymorphisms in venous thromboembolism is accepted and their role in arterial thromboembolism has come to be recognized in recent years.
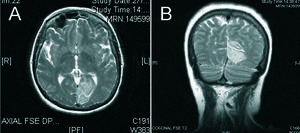
Woman aged 52 years, a smoker (tobacco and cannabis), and menopausal for 4 years. No relevant family history. Presented superficial thrombophlebitis 18 years previously. In 2001, following surgical treatment of hallux valgus, the patient developed deep vein thrombosis in the right lower extremity and was treated with ongoing acenocoumarol. In order to perform a thrombophilia workup, anticoagulant therapy was suspended and 2 months later, whilst awaiting results and not receiving treatment, the patient was admitted to our hospital with acute anterior myocardial infarction (AMI) and fibrinolysis was performed with tenecteplase. Following ST-segment normalization, the patient developed homonomous hemianopia as a result of an occipital infarction (Figure). Echo-Doppler of the supraaortic arteries and laboratory workup were normal, cholesterol concentration was 190 mg/dL (high-density lipoprotein cholesterol, 53 mg/dL; low-density lipoprotein cholesterol, 122 mg/dL), and the concentration of triglycerides was 75 mg/dL. Maximum troponin I levels were 104.7 ng/mL (normal, <0.20 ng/mL) and peak creatine kinase was 2934 U/L (normal, <215 U/L). The echocardiogram revealed mild ventricular dysfunction caused by anterior septal and apical hypokinesis along with the absence of thrombi. Coronary arteriography revealed irregularities in the anterior descending artery.
Thrombophilia workup confirmed protein C deficiency (assay type: chromogenic, 58%; clot, 32%; antigenic, 44%; normal values, >70%) and the presence of the C677T variant of the MTHFR gene in heterozygosis. The patient was treated with aspirin, acenocoumarol, and simvastatin and did not tolerate other medication for hypotension. At 12-month follow-up, the patient was only affected by the visual deficit.
This case is peculiar due to the recurrence of arteriovenous thrombosis in the presence of few classical risk factors and minimal angiographic lesions. This clinical profile may indicate the presence of genetic polymorphisms that favor thrombosis.3
Protein C deficiency predisposes for venous thromboembolism and has a prevalence in healthy adults of 0.5%.4 A recent report linked protein C deficiency with arterial thrombosis (AMI and stroke).5 Association with other factors such as smoking, cannabis use,6 or mutations in the gene for MTHFR, further predispose to thrombotic syndromes. The C677T polymorphism in MTHFR leads to an intermediate enzyme activity that is linked to hyperhomocysteinemia and arterial thrombosis.7,8 This patient had a history of recurrent venous thrombosis and presented AMI and ischemic stroke in the presence of these 2 prothrombotic factors.
Current data indicate that hypercoagulability must be ruled out in men aged up to 50 years and women up to 55 years with recurrent thromboembolism in the absence of arterial stenosis, with few risk factors, and without prothrombotic diseases or treatment, and/or with family history of thrombosis.2 Diagnosis of thrombophilia is important due to its therapeutic implications.