Keywords
INTRODUCTION
Percutaneous, epicardial, radiofrequency ablation is a non-surgical technique for treating ventricular tachycardia (VT). Its use has been described in patients with VT caused by Chagas disease and prior myocardial infarction, although rarely in patients with VT but with no structural heart disease.1-11
PATIENTS AND METHODS
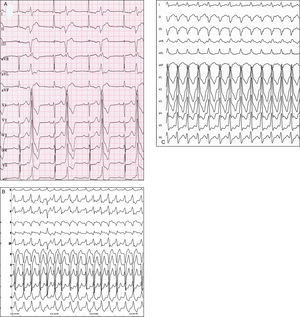
Over a period of 2 years, 34 patients with clinical VT (of which 14 showed no post-infarction scarring) were treated with radiofrequency ablation. In 3 patients a percutaneous epicardial approach was indicated since prior attempts at conventional endocardial ablation had failed. Table 1 shows the characteristics of these 3 patients. Patients 1 and 3 showed frequent, non-sustained ventricular tachycardia and monomorphic ventricular extrasystoles (practically incessant at rest and sustained during exertion; Figure 1). Patient 2 showed sustained monomorphic ventricular tachycardia (SMVT) during exercise (Figure 1). Prior to the epicardial procedure, the 3 patients were examined in the electrophysiology laboratory (after giving their signed, informed consent). Their anti-arrhythmia medication was suspended 5 half-lives before testing. Attempts were made to induce VT by programmed, basal, ventricular stimulation, and after the administration of isoproterenol.
Figure 1. Twelve-lead electrocardiogram during clinical arrhythmias in patients 1 (A), 2 (B), and 3 (C).
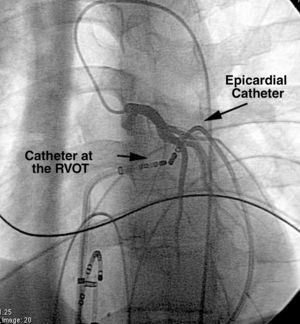
Transient success was obtained in all 3 patients during endocardial radiofrequency ablation using irrigated-tip catheters. However, after a period ranging from a few minutes to a few days, arrhythmia reappeared in all cases. Pericardial puncture was necessary in patients 1 and 2. This was performed using a needle 69.85 mm (2.75") in length, via which a guidewire (diameter 0.97 mm; 0.038") was introduced. The latter allowed an 8F introducer to be positioned directly--a change of guidewire is necessary when epidural needles are used. The remainder of the procedure has been previously described.1-4 In patient 3, the epicardial procedure was performed via a left posterior coronary vein belonging to the coronary sinus branch. Endocardial and epicardial mapping was performed using the CARTO system (Biosense, Webster). In patients 1 and 2, 7 F catheters with irrigated tips were used. Radiofrequency ablation lesions were induced at a power of 30-35 Watts, maintaining a temperature of 50oC. In patient 3, a 5F ablation catheter (Medtronic) was used since the small caliber of the vein precluded access with an irrigated-tip catheter. In this case, the temperature was maintained at 60ºC. Simultaneous coronary angiography was performed in all patients to avoid inducing ablation lesions in the coronary arteries. Following the procedure, the patients were treated with acetylsalicylic acid for 2 months. All patients underwent an echocardiogram, Holter monitoring and a stress test at 1, 3, and 6 months after the procedure.
RESULTS
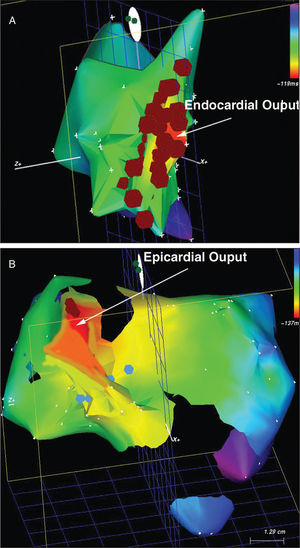
The VT mechanisms of all the patients were compatible with trigger activity: they were induced (although with poor reproducibility) after the infusion of isoprenaline, and with bursts of extrastimuli rather than single extrastimuli. The stimulation maneuvers showed re-entry not to be the mechanism of tachycardia. Epicardial pace-mapping was performed in all 3 patients during sinus rhythm, which reproduced the 12-lead electrocardiograms of clinical VT, although high stimulus output energies were required (10-15 Vx2 ms). In all 3 patients, earlier local electrograms (with respect to the QRS complex in VT) were achieved than with the prior endocardial procedure (Table 1). Before radiofrequency ablation, none of the patients showed abnormal endocardiac potentials in terms of duration or voltage. Coronary angiography showed patients 2 and 3 to have normal coronary arteries. Patient 1 had a 70% lesion in a poorly developed circumflex artery. This was not treated since it was believed to play no role in the etiopathology of the VT. In no case was it necessary to undertake ablation at less then 5 mm from an important coronary artery. Patient 2 underwent right ventriculography, magnetic resonance and right ventricular biopsy in order to exclude arrhythmogenic dysplasia. The endocardium and epicardium of the right ventricular outflow tract (Figures 1 and 2), the left ventricular outflow tract and the aortic root were unsuccessfully mapped in this patient. In patient 3, venography of the coronary sinus was performed. In all patients, VT similar to the clinical form was induced during the epicardial ablation procedure. No complications arose in any patient, although all referred to non-specific precordial discomfort after the procedure. At 24 h the patients' echocardiograms were normal and no pericardial rubbing was heard. No patient showed any sign of recurrence at one year of follow-up, and in patients 1 and 3 the left ventricular ejection fraction had normalized.
Figure 2. Activation maps of patient 1 obtained during clinical arrhythmia. A: Map obtained with the CARTO system for the endocardium of the right ventricular outflow tract. The red dots represent the failed attempts in this region. The arrow indicates the zone (red) where the earliest endocardial activation was seen during ventricular arrhythmia. B: Epicardial map showing where radiofrequency ablation was successfully performed. The arrow indicates the zone (red) where the earliest endocardial activation was seen during ventricular arrhythmia
Figure 3. Image of patient 1 showing the epicardial ablation catheter close to an endocardial ablation catheter in the region where treatment led to transitory success only. Note the relative proximity of the epicardial ablation catheter (in the area where treatment was successful) to the left descending coronary artery (simultaneous coronary angiography, left anterior oblique projection [15º]).
DISCUSSION
Conventional endocardial ablation failed to resolve the VT of these three patients, but the described epicardial approach was successful. The recent literature reports a number of small groups of patients to have been successfully treated in this manner.6-11 The novelty of the present report lies in the fact that, in patient 2, the tachycardia originated in the right ventricular outflow tract. The shape of the QRS complex of this patient during VT coincided with some features recently regarded as characteristic of an epicardial origin (slow initial QRS forces).6 Schweiker et al10 reported the origin of the VT to lie in the right ventricular outflow tract in only 1 patient of the 30 they subjected to epicardial mapping. However, this patient was successfully treated by the endocardial and not the epicardial route.
In patient 2, the reason why tachycardia could not be abolished from the endocardium of the right or left outflow tract, or even from the aortic root, suggests that the lesions produced by the radiofrequency ablation procedure where not transmural. This, however, does seem rather strange since the thickness of these regions is probably no greater than 1 cm. Alternatively, part of the VT circuit may have fallen within the region joining the septum to the anterior wall of the right ventricular outflow tract, thus rendering an epicardial approach the only one possible. In the other 2 patients, the VT circuit was in the epicardium in the posterio-inferior area close to the mitral annulus. In the study performed by Schweiker et al,10 the VT of 9 of the 30 patients was abolished by ablation in regions close and either anterolateral or posterolateral to the mitral annulus. However, although one patient presented with dilated cardiomyopathy, the authors did not report whether ventricular function improved after ablation. In the present study, patients 1 and 3 had frequent (practically incessant), non-sustained, monomorphic tachycardia. Both showed left ventricular dysfunction of no other possible cause than VT, and improved spectacularly after the ablation procedure. In our opinion, epicardial radiofrequency ablation should be considered in patients with ventricular dysfunction and very frequent monomorphic arrhythmias (especially if there is no other cause to justify such dysfunction), since the risks associated with the procedure are relatively small and the benefit that might be gained is great.
In the epicardial approach, ablation occurs close to the coronary arteries. Recent studies suggest this presents no complications.3 However, none of the present patients required ablation be performed within 1 cm of these arteries. The use of an irrigated-tip might increase the risk of damaging these vessels.
In conclusion, epicardial radiofrequency ablation can be curative and should therefore be attempted in patients with VT (but without heart disease) when the endocardial approach fails.12 It should even be attempted if the point of origin of the tachycardia lies within the right ventricular outflow tract. A diagnosis of tachycardiomyopathy should be considered for patients who present with dilated cardiomyopathy or very frequent, non-sustained, monomorphic VT, since ablation treatment can lead to the normalization of ventricular function.
Correspondence: Dr. J. Villacastín.
Unidad de Arritmias. Hospital Clínico San Carlos. 2.a Norte.
Prof. Martín Lagos, s/n. 28040 Madrid. España.
E-mail: jvillacastin@secardiologia.es