To the Editor,
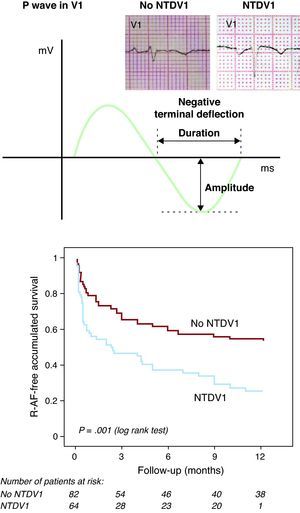
Approximately 30%-60% of patients who undergo cardioversion for atrial fibrillation (AF) suffer a recurrence (R-AF) in the mid-term.1 Among the different variables associated with R-AF, dilation of the left atrium (LA)2, 3 is probably among the best known. Little information exists, however, on the capacity of the morphology of the P wave to predict the probability of R-AF. The P wave reflects the electrical depolarization of the atrium. When it is biphasic in the precordial V1 lead, the negative terminal portion represents the electrical activation of the LA.4 An increase in its magnitude is associated with an increase in the volume of the LA, a delay in conduction, or both. We aimed to determine whether the presence of a negative terminal deflection of the P wave in V1 of ≥0.1mV and lasting ≥40ms (NTDV1) distinguishes patients at greater risk of R-AF following cardioversion for lone AF of recent onset (Figure 1).
Figure 1. Top: diagram showing measurement of the negative terminal deflection of the P wave in V1. Bottom: recurrence of atrial fibrillation after cardioversion. Kaplan-Meier curves. NTDV1: negative terminal deflection of the P wave in V1 of ≥0.1mV and lasting ≥40ms; R-AF: recurrence of atrial fibrillation.
Between January 2006 and March 2007, we undertook a prospective study of 146 consecutive patients with lone AF of recent onset (<48h) that was reverted to sinus rhythm (SR) at our center: in 61 patients (42%) the AF episode ended spontaneously; 85 patients (58%) required either electrical (n=38) or pharmacological cardioversion (n=47). No patient suffered ventricular dysfunction nor any significant valve disease. Table 1 shows the baseline characteristics of the patient population. Follow-up was undertaken for one year. R-AF was defined as a clinical recurrence (the perception of an arrhythmic pulse lasting more than 1min) or an electrocardiographic recurrence detected during programmed or additional appointments during follow-up.
Table 1. Univariate Analysis of the Predictors of Recurrent Atrial Fibrillation (Log Rank Test).
| Variable | Value for the entire sample, no. (%) | R-AF (%) a | Log rank (χ2) | P |
| Age>75 years | 40 (27) | 40 vs 56 | 0.43 | .51 |
| Men | 93 (53) | 56 vs 59 | 0.11 | .74 |
| High blood pressure | 90 (61) | 57 vs 57 | 0 | 1 |
| Diabetes mellitus | 21 (14) | 52 vs 58 | 0.62 | .43 |
| Persistent AF | 85 (58) | 59 vs 56 | 1.16 | .28 |
| Treatment with anti-arrhythmia medication b | 56 (38) | 50 vs 62 | 1.51 | .22 |
| ACEI/ARB-II | 77 (53) | 55 vs 61 | 1.54 | .22 |
| Creatinine clearance<60 ml/min | 18 (12) | 78 vs 55 | 6.92 | .01 |
| Area of LA ≥20 cm2 | 85 (54) | 65 vs 48 | 6.8 | .01 |
| NTDV1 | 65 (44) | 72 vs 46 | 11.55 | .001 |
ACEI, angiotensin converting enzyme inhibitors; AF, atrial fibrillation; ARB-II, angiotensin II AT1 receptor antagonists; LA, left atrium; NTDV1, negative terminal deflection of the P wave in V1 of ≥0.1mV lasting ≥40ms; R-AF, recurrent atrial fibrillation.
a Percentage of patients with recurrent AF after cardioversion (present vs absent).
b Twenty-eight patients were treated with amiodarone and 28 with flecainide.
All calculations were performed using SPSS/PC v.17 software (SPSS Inc.; Chicago, Illinois, United States). Continuous variables with a normal distribution were described as means±standard deviation; continuous variables not showing a normal distribution were expressed as medians [interquartile range]; categorical variables were expressed as absolute numbers and percentages. These different groups of variables were analyzed using the Student t test, the Mann-Whitney U test and the χ2 test respectively. The log rank method was used for the univariate analysis of survival. The independent predictors of R-AF during follow-up were determined via Cox regression analysis including the following variables: age >75 years, male sex, high blood pressure, diabetes mellitus, persistent AF, treatment with type II or III anti-arrhythmia drugs (AAD), angiotensin converting enzyme inhibitors/angiotensin II receptor AT1 antagonists, creatinine clearance <60ml/min, area of the LA in apical four chamber plane (cm2), and NTDV1. Significance was set at P<.05.
After 1 year of follow-up, 84 patients (58%) suffered R-AF. Table 1 shows the relationship between the different variables and the frequency of R-AF. Sixty five (46%) patients showed NTDV1 after the recovery of SR, although this was significantly more prevalent in patients with persistent AF (52% compared to 34%; P=.044). R-AF was more common in patients with NTDV1 (73% compared to 46%; P=.001) (Figure 1). Cox regression analysis showed the independent predictors of R-AF to be: NTDV1 (odds ratio [OR]=1.9; P=.007), LA area (OR=1.1; P<.001) and treatment with AAD (OR=0.52; P=.013). NTDV1 was associated with a greater incidence of R-AF in patients with a non-dilated LA (64% compared to 39%; non-adjusted P=.02) and in those with an LA area of ≥20cm2 (77% compared to 53%; non-adjusted P=.04).
This study shows that, in patients with no structural heart disease, the presence of NTDV1 is independently associated with an increase in the risk of R-AF in the first year following cardioversion to recover SR. The slowing down of electrical conduction, the pressure and/or volume overload of the LA, and structural changes (such as dilation or hypertrophy) all increase the magnitude of the terminal deflection of the P wave in V1.5, 6 These factors have all been related to the development of changes in the histological and electrophysiological characteristics of the LA5 and may therefore favor R-AF after the recovery of SR. It is assumed that in patients with AF, electrical abnormalities precede anatomical changes. Although we observed that NTDV1 was more common among patients with a dilated LA, the association between NTDV1 and R-AF was independent of the size of the atrium size. This might indicate that this association defines a relatively early delay in atrial conduction, earlier sometimes than the dilation of the LA.
Given the type of follow-up pursued, in which long periods elapsed without electrocardiographic monitoring, R-AF might have been underestimated since many recurrences are asymptomatic. Finally, neither the duration of episodes nor the prior arrhythmic load were included in the statistical analysis (although in all patients AF lasted less than 48h). Their inclusion may have provided extra information.
.
Corresponding author: jimenezcandil@secardiologia.es