The femoral artery is the access site of choice for the ablation of cardiac arrhythmias with a retrograde aortic approach, such as idiopathic ventricular arrhythmias or those associated with scar tissue or specific left-sided accessory pathways. However, the proximal portion of the aorta cannot always be reached via this access site.
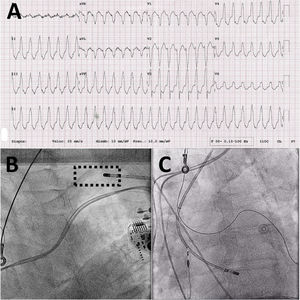
We present the case of an 89-year-old man with a history of anteroapical myocardial infarction who had undergone dual-chamber pacemaker implantation due to complete atrioventricular block and who had aortoiliac occlusive disease treated with aortocoronary surgery 40 years previously. The patient presented to the emergency department due to asthenia. Upon arrival, he was found to have hypotension and tachycardia. Electrocardiography was performed, showing regular wide QRS tachycardia with an inferior axis at 176 bpm, compatible with sustained monomorphic ventricular tachycardia originating in the region of the outflow tracts. A V3 transition with a positive QRS complex in lead I and QS morphology in V1 with notching in the descending branch of the QRS complex suggested a likely successful approach from the aorta1 (figure 1A). Termination was unsuccessfully attempted using overdrive pacing from the ventricular pacemaker lead, which was followed by attempted electrical cardioversion with a biphasic synchronized shock at 200J. However, the tachycardia was incessant, with an almost immediate relapse after 3 cardioversion attempts. Accordingly, intravenous perfusion of amiodarone was begun, which slowed the tachycardia to 155 bpm without stopping it. Electrical cardioversion was attempted 3 times, but the incessant behavior remained. Given the hemodynamic impact and the impossibility of stopping the tachycardia using conservative strategies, emergency ablation was indicated.
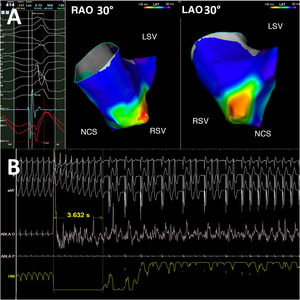
Both femoral arteries were cannulated with the aid of a guidewire but we were unable to reach the abdominal aorta. Accordingly, angiographic probes were used, which confirmed the complete bilateral occlusion of the aortoiliac arteries. A possible approach from the right ventricular outflow tract was not completely ruled out. However, we decided to attempt a retroaortic approach, even though it would involve a less conventional strategy, because its speed would avoid hemodynamic deterioration and the possibility of complications related to the use of radiofrequency in the right ventricle,2 given that the electrocardiographic pattern was highly compatible with a mappable origin in the right sinus of Valsalva or the commissure between the right and left sinuses. Ultrasound-guided access was obtained via the left axillary artery (video 1 of the supplementary data) with an 8-Fr Avanti+ introducer (Cordis, Cardinal Health, United States), and a ThermoCool SmartTouch contact forcesensing irrigated ablation catheter (Biosense Webster, United States) was advanced to the aortic root (figure 1B,C). Activation mapping performed with the CARTO3 electroanatomic mapping system (Biosense Webster) revealed greater precocity of the ventricular electrogram in the right sinus of Valsalva, whose bipolar signal also showed a prepotential that preceded the QRS onset by 29ms, in addition to an electrogram with QS morphology in the monopolar signal (figure 2A). A 50-W application to this area terminated the tachycardia in 3.6seconds (figure 2B); another 5 adjacent applications were applied as backup. After a 30-minute evaluation period in which we failed to observe arrhythmia recurrence or to induce tachycardia with ventricular pacing protocols (with trains and up to 3 extrastimuli, as well as ramps, with a minimum cycle length of 200ms), the introducer was extracted and hemostasis of the puncture site was performed via application of an Angio-Seal vascular closure device (St Jude Medical, United States). Vascular ultrasound on the following day ruled out complications at this location.
A: electroanatomical activation mapping of the aortic root in 2 views that shows the maximum precocity in the RSV. B: polygraphic recording during radiofrequency application with termination of the tachycardia at 3.6seconds. LAO, left anterior oblique; LSV, left sinus of Valsalva; NCS, noncoronary sinus; RAO, right anterior oblique; RSV, right sinus of Valsalva.
Transfemoral arterial access can be limited in 13% to 20% of patients due to prior vascular interventions, severe aortoiliac atherosclerotic disease, and major calcification or tortuosity.3 Given the current growth in the older population affected by tachyarrhythmia, increases are expected in the number of patients with these comorbidities and the impossibility of a conventional approach via the femoral artery. Although transseptal access to the left ventricle can help to avoid this problem, mapping and ablation of the anterior wall or aortic root using this approach is often complicated due to insufficient maneuverability,4 which can lead to worse outcomes and major complications. A previous publication has already reported successful ablation of ventricular tachycardia via a 6-Fr radial artery access site with a 4-mm nonirrigated tip.5 However, the reduced diameter of this artery impedes the use of larger-caliber introducers and, thus, conventional irrigated ablation catheters. Axillary artery access has been proven to be a valid alternative in cardiac interventions and permits transcatheter aortic valve implantation and establishment of mechanical circulatory support but is not without risks. The main complications are insertion site bleeding and hematoma (≈10%). Less frequent are the development of pseudoaneurysm, dissection, thrombosis, and upper extremity ischemia, which have been linked to larger-caliber access sites and prolonged intervention times, generally related to mechanical circulatory support. Given the extrathoracic nature of the axillary artery, correct insertion, preferably in its second segment, reduces the possibility of other potentially severe complications related to subclavian access, such as pneumothorax and hemothorax.3 The use of ultrasound is recommended to improve success and reduce complications. Hemostasis can be complex, and vascular closure devices are often used, although manual compression of the second rib is a valid alternative for access sites < 9 Fr in diameter in nonanticoagulated patients. To conclude, this is the first reported case of the successful ablation of ventricular tachycardia using an ultrasound-guided axillary artery approach.
This work has been conducted in accordance with international recommendations on clinical research and has been approved by the institutional ethics committee. Informed consent was obtained from the patient in question.
FUNDINGThe present work did not receive any funding.
AUTHORS’ CONTRIBUTIONSC. Lozano Granero wrote the manuscript. All of the authors have substantially contributed to the design, data collection, analysis, and interpretation, critical revision of the intellectual content, and approval of the final version.
CONFLICTS OF INTERESTNone of the authors declare conflicts of interest in relation to the content of this manuscript.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2023.02.007