Keywords
HISTORICAL DEVELOPMENT
The aim of this section is firstly to explain the medical reasons for the appearance of a "minimally invasive revolution" that, without any doubt, addresses a problem in the field of coronary artery bypass surgery, and secondly, to review the current status and results obtained with the various technical alternatives that have arisen.
The Birth: "Adapt and Evolve or Die"
Coronary revascularization surgery was initially performed on the beating heart. This led to a variety of significant problems: on the one hand, the movement of the vessel to be sutured significantly compromised the reliability of the anastomosis, while on the other, the blood flow in the vessel itself or the collateral circulation hindered visibility, and finally, in order to reach specific branches on the lateral or posterior surface of the heart, it was necessary for the heart to be dislocated or displaced, resulting in hemodynamic deterioration.
Probably the most important step in the development of current coronary surgery was the use of extracorporeal circulation, initiated by Gibbon in 1953, since it made it possible to perform coronary surgery on an organ that is stable, free of blood, and that can be freely manipulated in order to expose any coronary vessel. Another essential step in the development of this type of surgery was the introduction of coronary angiography by Sones and Shirey. For the first time, it became possible to define and quantify coronary obstructions in vivo and assess their impact on patient prognosis.
Various factors have been found to be involved in the morbidity and mortality associated with coronary artery bypass grafting; these include pathophysiologic changes triggered by the use of extracorporeal circulation, ischemic damage occurring during cardioplegia, hypothermia, and median sternotomy. Despite these various considerations, with the exception of myocardial protection, the essential surgical strategy has not changed in the last 25 years. Of particular importance in relation to morbidity are neurological complications, reported by Roach et al1 to occur at a rate of 6.1% in a prospective multicenter study that included 2108 patients. These complications are attributable to emboli arising from atheroma plaques due to manipulation of the ascending aorta, to microemboli, or to reduced cerebral perfusion pressure during cardiopulmonary bypass. The tendency to operate on ever older patients makes these complications increasingly likely. Roach et al1 concluded that "Adverse cerebral outcomes after coronary bypass surgery are relatively common and serious; they are associated with substantial increases in mortality, length of hospitalization, and use of intermediate-term or long-term care facilities. New diagnostic and therapeutic strategies must be developed to lessen such injury."
At the beginning of the 1990s, 2 surgical strategies came together to facilitate the development of new therapeutic opportunities in coronary surgery. Firstly, for largely socioeconomic reasons, off-pump coronary surgery had been successfully performed for more than 10 years in selected patients at some hospitals in South America.2-6 At the same time, video-assisted and minimally invasive surgical techniques that were already in use in other fields also began to be applied to the chest cavity. Thorascopic surgery inspired the development at Stanford University in 1991 of video-assisted coronary artery bypass surgery with limited thoracotomy and cardioplegia, so-called "port access" coronary artery bypass grafting. However, it is worth pointing out that extracorporeal circulation and cardioplegic arrest of the heart continue to be a fundamental aspect of the Stanford strategy and, consequently, the morbidity arising from these procedures is not eliminated.7,8
Coronary revascularization surgery has also been influenced by the development of percutaneous coronary interventions. The widespread use of balloon angioplasty and the introduction of the stent for the reduction of restenosis have led to significant quantitative and qualitative changes in the case mix of coronary artery bypass surgery. The availability of a therapy that exhibits very low morbidity and mortality and good short-term clinical results, but that has a substantial incidence of restenosis and requirement for repeat revascularization in the short term and with unknown clinical and angiographic results in the medium and long term (>3-4 years), meant that coronary surgery had to evolve in 2 directions: on the one hand, aiming for maximum durability through an extension of arterial revascularization and the intraoperative use of high-magnification stereo microscopes (magnification, x5.5), and on the other, with a reduction of surgical invasiveness that allows better and faster recovery in low-risk patients, a reduction in morbidity and mortality in high-risk patients, and even the treatment of patients who were previously considered inoperable. Clearly, the quality of the intervention cannot be compromised in an effort to achieve the second objective, since the durability of the procedure would be affected.
A Terminology Problem
The terminology used in the last decade is extremely confusing, perhaps due to deliberate misuse of the term "minimally invasive." The concept of the "invasiveness" of a surgical technique is intimately linked to the morbidity that it generates. As mentioned, there are 3 sources of morbidity in conventional coronary artery bypass surgery, each of which has a specific weight according to the individual characteristics of the patient: median sternotomy, extracorporeal circulation, and manipulation of the aorta. The following would be alternatives to make the surgery less invasive, in other words, to reduce the associated morbidity: reduce incisions by searching for alternatives to median sternotomy, eliminate the use of extracorporeal circulation, and do not manipulate the aorta, either for cannulation or as an origin for bypass grafts. The practical application of these ideas has led to a wide range of alternative, "less aggressive" techniques:
1. Off-pump coronary artery bypass grafting (OPCABG).
2. Off-pump coronary artery bypass surgery via minimal incisions, known under the generic term MIDCABG (minimally invasive direct coronary artery bypass grafting), within which various different approaches have been described: right and left parasternal, right anterior minithoracotomy, and the most widely used route for which the most extensive clinical experience has been obtained, directly visualized left anterior minithoracotomy to suture the internal mammary artery (IMA) to the anterior descending artery, known as the CABG-LAST (coronary artery bypass grafting left anterior small thoracotomy) operation.
In this group, the dissection of the IMA is performed partially or totally under direct visualization, or completely using video-assisted techniques.
A variant of the technique developed following the increasing use of MIDCABG is known as "hybrid" revascularization9,10 and consists of revascularization of the anterior descending artery through minimally invasive surgery and of the remaining vessels via percutaneous coronary angioplasty. Given the development, reliability, and safety achieved with off-pump techniques performed via median sternotomy, approaching all areas of the heart, even in high-risk patients, it is our opinion that hybrid revascularization should be considered a second choice alternative, limited to exceptional cases.
3. Port-access CABG, in which femorofemoral extracorporeal circulation is used with cardioplegia via left anterior small thoracotomy, similar to the previous group.
The advantages and disadvantages of each of these techniques are compared with conventional coronary artery bypass grafting in Table.
Consolidation: From the Adventure to the Organized Tour
In the second half of the 1990s significant technological developments were made that sought to address the technical barriers to performing off-pump surgery. These included the appearance of various epicardial stabilizers to reduce regional movement, intracoronary shunts to facilitate perfusion during anastomosis, blowers to keep the anastomosis area free of blood, positioners to aid dislocation of the heart, flow measurement apparatus to guarantee the quality of the anastomosis, and specific surgical instruments.11-14 At this point, we begin to move from "artisan" off-pump coronary artery bypass grafting, based on a huge weight of experience and ability on the part of the surgeon, a large amount of improvisation, and poor reproducibility, to regulated and protocol-based surgery that guarantees the quality of the results and the use of the technique in more patients and by more surgeons.
Off-pump coronary artery bypass grafting performed via median sternotomy is not an adaptation of the conventional technique, although both involve the manipulation of coronary arteries, use of saphenous vein or arterial bypass grafts, and the construction of an anastomosis between the two. The 2 modalities differ in their knowledge base, logic, and the techniques involved. Thus, undertaking off-pump surgery requires specific learning and training that must be undertaken rigorously in order to achieve the desirable results. This has represented one of the main barriers to increasing the use of the technique.
To our knowledge, 2 technical issues have been determining factors in the development of protocol-based off-pump coronary artery bypass grafting: learning how to manipulate and expose the heart and reduce heart movement, and monitoring of graft patency by intraoperative Doppler.
Exposure and Regional Reduction of Cardiac Movement
The renewed interest in coronary artery bypass surgery on the beating heart has led to the evaluation of a number of different possibilities and devices for the reduction of "global" or "regional" cardiac movement.
Initially, beta-blockers were used to reduce heart rate and even adenosine bolus was employed to generate cardioplegia, used to facilitate suturing.
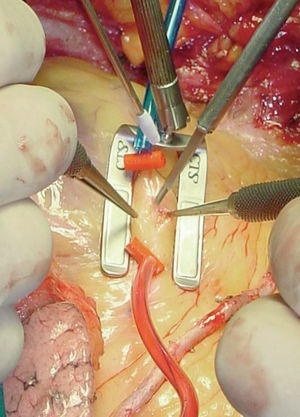
Subsequently, local stabilization devices, which allow the rest of the heart to beat under more physiologic conditions, have been developed for use in the region of the anastomosis; these devices are known under the generic term "epicardial stabilizers." Of the many commercially available devices, some act essentially through regional compression of the heart, of which the most widely used is the Guidant OPCABG system (Figure 1), and others immobilize the epicardium by suction on the tissue, notably the various versions of the Octopus (Medtronic Inc, Minneapolis, MN, USA; Figure 2).
Figure 1. Guidant Ultima regional stabilization device, which works through pressure. Position to perform anastomosis to the anterior descending coronary artery. The figure shows the arterial occlusion sutures and the dissection of the artery.
Figure 2. Octopus stabilization device, which works through the use of suction. Position to perform anastomosis to the anterior descending coronary artery with the internal mammary artery.
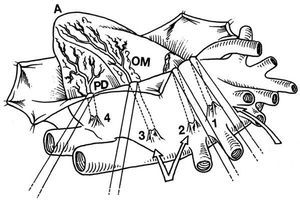
These devices and the use of pericardial traction sutures, or a cotton sling in the transverse sinus, facilitate the rotation and displacement of the heart that is necessary to access the vessels on the lateral and posterior surface (Figure 3).13,14
Figure 3. Dislocation of the heart using pericardial traction sutures to expose the lateral and inferoposterior surface. "Lima sutures." Taken from Baumgartner et al.44
Qualitative and Quantitative Assessment of Anastomosis: Measurement of Flow in Bypass Grafts by Intraoperative Doppler
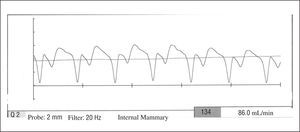
The surgical technique that we want to develop could, due to its complexity, compromise results in terms of graft patency. Given that we have an alternative technique, on-pump surgery, which has good demonstrated results in the short and long term, we believe that assessment of each anastomosis is obligatory in off-pump surgery (Figure 4).15-21
Figure 4. Intraoperative measurement of flow in the bypass graft.
The change in blood flow pattern seen in grafts when they are anastomosed to the heart, with a reduction in the systolic wave and the appearance of a predominant diastolic wave, allows us to undertake a qualitative assessment of patency (Figure 5). In addition, commercially available equipment can be used to obtain various quantitative measurements of flow and indices, the most widely used being average flow rate and pulsatility index (patency <3). When assessing anastomosis patency, we should always place greater emphasis on the presence of a predominant diastolic wave in the flow, since the quantitative value of the flow is influenced by the caliber of the vessel and the extent of stenosis in the coronary artery, which can lead in some cases to competitive flow.
Figure 5. Flow in the bypass graft obtained using an intraoperative flowmeter. The figure shows the presence of a predominant diastolic wave, providing qualitative information on patency.
INDICATIONS
Indications for off-pump surgery are under constant revision because of the influence of improvements in immobilization techniques that, on the one hand, extend the number of patients who can undergo this type of surgery but, on the other, imply modification of the indications according to the short-term and long-term results obtained. The results obtained with off-pump surgery in the era prior to the advent of stabilizers were suboptimal, largely due to deficient technical results and incomplete revascularization.
Any patient who is a candidate for traditional surgery is amenable to treatment by off-pump surgery. In the preoperative assessment, only ventricular function and unstable angina should alert us to difficulties in exposing the lateral and inferior surface of the heart. However, experience has demonstrated that following revascularization of the anterior surface, which requires minimal distortion, sufficient hemodynamic stability is obtained to allow the remaining areas to be approached. Consequently, the preoperative condition of the patient does not exclude them from off-pump surgery; furthermore, such patients will obtain the greatest potential benefit from the use of this technique.
Attention has been drawn to certain anatomical characteristics that cause difficulty in performing off-pump surgery; these include extensive calcification, myocardial bridging, and small-caliber vessels. Although these characteristics must be taken into account in surgery performed via left anterior small thoracotomy, after a surgeon has undergone a period of training, they should not be considered absolute contraindications if the surgical approach is via median sternotomy.
Initial data from some surgical teams and individual surgeons indicate that it is possible to perform 75% to 98% of all coronary artery bypass grafting without extracorporeal circulation, figures which would lead to a substantial reduction in costs and the use of health resources for heart surgery.22-32 On a world scale, it is calculated that 20% to 30% of coronary artery bypass surgery is performed off pump; in some countries the proportion is greater than 50% and in some hospitals up to 98% of unselected cases are treated in this way.
In our group, the surgical technique of choice for myocardial revascularization is currently off-pump double arterial revascularization with IMAs. Therefore, this type of surgery is planned for all patients from the outset. In our experience, intraoperative ischemia that does not respond to medical treatment and use of an intraaortic balloon pump is the only situation that can make it impossible to do without extracorporeal circulation.
OFF-PUMP CORONARY ARTERY BYPASS SURGERY: NEW ISSUES IN ANESTHETIC AND POSTOPERATIVE MANAGEMENT
Reducing Surgical Aggression: More Than Just Eliminating Extracorporeal Circulation
A program of off-pump cardiac surgery requires adequate multidisciplinary intraoperative and postoperative planning in order to achieve certain clearly defined objectives. Our aim is not only to achieve a reduction in the aggression for the patient that may lead to a reduction in morbidity and mortality but also to accelerate the surgical process, thereby allowing a reduction in the use of hospital resources (mainly time in critical-care beds), cost, and the recuperation period of the patient.
Unlike with on-pump cardiac surgery, where the role played by the anesthetist has little effect on the final results, the training and experience of the anesthetist is a determining factor in obtaining the best results with off-pump coronary artery bypass grafting, both during surgery and in the postoperative period.
Heart surgery carries with it certain specific considerations regarding anesthesia; these can be defined in terms of prevention of myocardial ischemia, maintenance of anesthetic depth, hemodynamic stability, reduced response to surgical stress, and planning of postoperative care.
Choice of Anesthetic Technique
The choice of any anesthetic technique is affected by the objectives of the procedure. Anesthetic management during off-pump surgery includes the general characteristics of any anesthetic procedure--analgesia, amnesia, hypnosis, and immobilization--at the same time as providing maximum hemodynamic stability during manipulation of the heart and myocardial protection during coronary clamping. However, this anesthetic management becomes increasingly complex when the aim is for the patient to wake as quickly as possible without postoperative pain.33-46
Multimodal Anesthesia
In recent years, multimodal anesthetic techniques have been introduced to the field of heart surgery. These involve a combination of regional and general anesthesia in an attempt to reduce the response to surgical stress, without a requirement for high-dose opioids, and provide excellent analgesia in the intraoperative and postoperative periods.33-35
Thoracic epidural anesthesia combined with general anesthesia. The benefits of these techniques are a reduction in myocardial oxygen demand as a result of reduced vascular resistance, heart rate, and sympathetic response to surgical stimulation. Other beneficial effects are an increase in myocardial and splanchnic perfusion caused by the sympathectomy produced in the thorax and a reduction in the response to surgical stress. Patients receiving epidural anesthesia have been shown to have lower levels of adrenaline, glucose, cortisol, and noradrenaline compared with patients anesthetized with high doses of fentanyl. The greater development of multimodal anesthesia is not only due to its advantages in relation to cardiac physiology but also due to it being an ideal technique for analgesia and ventilatory physiotherapy in the postoperative period.
This is the technique of choice if the patient is to be extubated at the end of the intervention.
General anesthesia combined with intrathecal opioids. The aim of administering intrathecal opioids is to provide intense anesthesia during the preoperative period through administration of a single dose (generally 0.3-0.5 mg morphine) prior to surgery. There are fewer advantages to the technique when compared with epidural anesthesia since it does not produce thoracic sympathectomy or selective analgesia; nevertheless, the analgesia is adequate. Another drawback is that the central side effects of opioids--mainly respiratory depression--can delay awakening, ambulation, eating, and discharge of the patient.
General anesthesia with peripheral nerve block: intercostal, interpleural, or paravertebral. This involves a combination of light general anesthesia and sensitive unilateral nerve block that produce excellent intraoperative and postoperative analgesia in those cases in which surgery is performed via lateral thoracotomy (anastomosis of a single vessel, anterior descending or right coronary artery).
General Anesthesia
Recently, the introduction of remifentanil, an ultrashort- acting opioid with intraoperative pharmacodynamic characteristics that come close to an ideal opioid, has created an opportunity to change the induction and maintenance techniques for cardiac anesthesia. The intraoperative use of this opioid allows anesthesia to be performed that is based mainly on analgesia and that is without risk of prolonged ventilatory depression. The pharmacological interaction with inhaled and intravenous drugs allows the dose of hypnotic drugs with vasodilatory or negative inotropic effects to be reduced. This favors hemodynamic stability and reduces the adrenergic and sympathetic response to surgical stress. The main drawback of remifentanil is in the treatment of postoperative pain, since the patient receives no residual analgesia following withdrawal of the drug. Epidural or intradural combined analgesia, preventative analgesia, and the combined administration of nonsteroidal antiinflammatory drugs and opioids are more effective in controlling postoperative pain than administration of opioids alone.36
Hemodynamic Monitoring and Management
Anesthetic monitoring is no different from standard monitoring in cardiac surgery: 3- and 12-lead electrocardiogram, pulse oximetry, capnography (graph of CO2 elimination), invasive arterial pressure monitoring, and monitoring of central venous pressure or pulmonary arterial pressure. The introduction of esophageal Doppler ultrasound, continuous cardiac output catheter, or assessment of SvO2 are useful for monitoring changes in cardiac output that can be caused by changes in the position of the heart and/or patient and can reduce mesenteric and/or cerebral ischemia.
Transesophageal echocardiography allows visualization of the heart chambers during the different phases of the intervention and, therefore, can guide positional changes.
Hemodynamic changes occur mainly due to a reduction in preloading of the left ventricle caused by compression of the right ventricle during manipulation of the heart; a Trendelenburg position of 30o to 40o usually restores preloading and output. Low doses of ephedrine or adrenaline are commonly administered to restore cardiac output and mean arterial pressure in those situations in which positional changes are not fully effective.
Myocardial Protection and Anesthesia
The anesthetic techniques mentioned provide some degree of myocardial protection--from a traditional perspective--by reducing myocardial oxygen consumption and improving oxygen delivery. These techniques reduce heart rate and left ventricular afterload, cause coronary vasodilation leading to improved collateral flow, and with appropriate hemodynamic management, can improve myocardial perfusion pressure. Administration of esmolol (an ultrashort-acting beta-blocker) during the intraoperative period helps reduce heart rate and myocardial oxygen consumption during coronary revascularization; low doses of this drug are of particular use when anesthetics are employed that do not produce bradycardia. Calcium antagonists such as diltiazem (5-10 mg/h) and nicardipine (0.4-0.6 mg/h), which exert an antianginal and spasmolytic effect on the coronary vessels, are also commonly used. Nevertheless, better myocardial protection against ischemia can be provided if certain characteristics of volatile anesthetics are understood; thus, it has been demonstrated that one or more periods of ischemia and reperfusion extend the tolerance of the myocardium to ischemia (ischemic preconditioning). Recent findings indicate that KATP channels and adenosine A1 receptors modulate an acute memory phase that prolongs tolerance to ischemia. Volatile anesthetics exert cardioprotective effects during ischemia-reperfusion through a mechanism of action that is similar to preconditioning (ischemia for 3 min followed by reperfusion) and some additive effects in tolerance of ischemia have been shown in animal studies.
Planning of Postoperative Care
The planning of postoperative care begins at the moment the patient enters the operating theater; certain factors, such as prevention of hypothermia (warming of intravenous fluids, temperature of the operating theater, active warming of the patient, etc), use of an appropriate anesthetic technique to allow extubation immediately after surgery or a few hours later in the recovery room, and excellent analgesia are details that, if forgotten, prevent early extubation, physiotherapy, and ambulation.
Prophylaxis of supraventricular arrhythmias does not differ from that performed with on-pump surgery and should be initiated during surgery. Although calcium antagonists and magnesium sulfate are often used for that purpose, administration of beta-blockers is currently one of the most common practices. The availability of esmolol allows beta-blockers to be used until those drugs can be administered orally, with the peculiarity that if they lead to low output the effects are transient following suspension of the treatment.
OFF-PUMP CORONARY ARTERY BYPASS GRAFTING WITH DOUBLE INTERNAL MAMMARY ARTERIES
Reducing Morbidity in Coronary Artery Bypass Grafting: Our View of the Problem
As mentioned in the previous section, reducing surgical aggression in coronary artery bypass grafting involves more than simply taking a patient off the cardiopulmonary bypass pump. Surgery must be planned with 2 goals: to eliminate or reduce all sources of morbidity and to seek the best early and late graft patency through the extensive use of arterial grafts.
In our opinion, to genuinely reduce the morbidity and mortality associated with on-pump myocardial revascularization surgery requires not only the omission of cardiopulmonary bypass but also the omission of side clamping of the aorta and the need to use saphenous veins. Furthermore, the anesthetic management of these patients should favor early extubation as an essential step towards reducing postoperative morbidity.
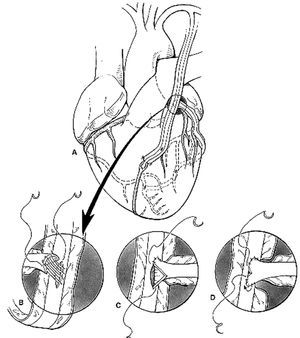
This reasoning is reflected in our technique of choice for coronary artery bypass grafting: total arterial myocardial revascularization with double IMA grafts, used as Y or T grafts (technique described by Tector et al48,49) performed without cardiopulmonary bypass (Figure 6).
Figure 6. Diagram showing revascularization with both internal mammary arteries (IMA) as a T graft. The left IMA is used to revascularize the anterior surface and the right IMA for the lateral and inferior surfaces of the heart. Taken from Tector et al.48,49
Off-Pump Coronary Artery Bypass Grafting With Double Internal Mammary Artery Grafts: Surgical Technique
Both IMAs are dissected as skeletonized arteries (without fascia, veins, or muscle) under a stereo microscope (magnification, x3.5-x5.5) in an effort to preserve the vasculature of the sternum, improve the length and caliber of the artery, and aid the construction of a T graft and sequential anastomoses. We perform sufficient heparinization, initially at 1.5 mg per kg body weight, to achieve an activated clotting time of more than 300 seconds, and this level is maintained throughout the entire period during which arterial occlusions are performed. Both IMAs are irrigated with warm physiologic saline and saline containing papaverine at a ratio of 1:30, without intraarterial pharmacological manipulation. The target coronary arteries are explored and the surgical strategy confirmed.
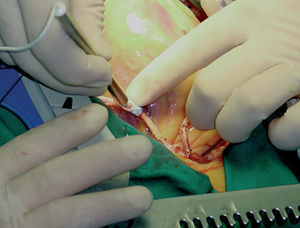
After dividing the proximal portion of the right IMA with metallic clips, the graft is constructed in a T (perpendicular end-to-side anastomosis) or Y configuration (parallel end-to-side anastomosis), according to the surgical plan, suturing the free right IMA graft to the left IMA at the level of the left atrial appendage, after exposing it via a lateral incision in the pericardium. The end-to-side anastomosis, around 8 mm in length, is prepared using a continuous suture with 8-0 nylon and pulsatility or flow is confirmed in both branches of the graft (Figure 7). In some cases it has been necessary to construct a second Y graft using a small segment of the left or right IMA, 2 to 4 cm in length, to a more distal portion of the left IMA in order to revascularize diagonal branches that run almost perpendicular to the anterior descending artery.
Figure 7. End-to-side anastomosis in parallel ("Y") between the right internal mammary artery (IMA) as a free graft and the left IMA.
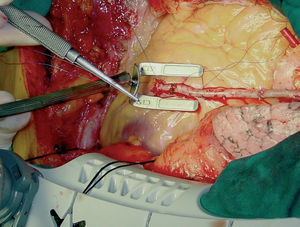
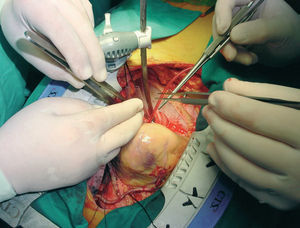
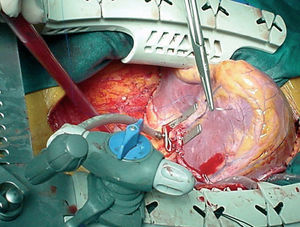
We always begin with the revascularization of the anterior surface of the heart, starting, if necessary, with the diagonal arteries and followed by the anterior descending artery (Figure 8). Subsequently, anastomoses are performed on the lateral (Figure 9), posterolateral, and inferior (Figure 10) surfaces, in that order. Although in the majority of patients revascularization of the anterior descending artery has been performed with the left IMA, in some, those in whom a longer or higher quality graft to this area is required, use of the right IMA has been preferred.
Figure 8. Completed anastomosis of a skeletonized left internal mammary artery to the anterior descending coronary artery performed without extracorporeal circulation using a Guidant Ultima stabilizer.
Figure 9. Exposure, stabilization, and sequential anastomosis of the right internal mammary artery to the second marginal branch. Verticalized position of the heart.
Figure 10. Exposure, stabilization, and terminal anastomosis of the right internal mammary artery to the posterior descending artery. Extreme verticalized position of the heart (apex towards the head of the patient).
In the former group, the strategy for exposure of the coronary arteries was based on the use of 4 cotton slings: 2 are passed through the transverse sinus and the other 2 underneath the inferior vena cava. Subsequently, we have modified the technique for elevation and rotation of the heart to access the lateral, posterolateral, and inferior surfaces of the heart, adopting the method described by Lima.49 This is based on the use of 2 to 3 silk stitches to elevate the left side of the pericardium, the first above the left superior pulmonary vein, the second close to the left inferior pulmonary vein, and the third in the vicinity of the inferior vena cava. Alternate or simultaneous traction on these stitches facilitates elevation and rotation of the base of the heart to the right and placement of the apex outside the thorax. Recently, some groups have simplified this maneuver by only placing cotton slings that pull on the transverse sinus or through the use of suction devices (positioners) at the apex. This position creates difficulties in filling of the right ventricle that are compensated by a Trendelenburg position of 20o, through which adequate hemodynamic stability is achieved. Over the years, we have used various stabilizers that have appeared on the market with improvements in technology, and we are currently using the CTS Ultima and the Octopus-3.
Once adequate exposure and stabilization of the target coronary artery is achieved with a good hemodynamic status, occlusion of the coronary artery is undertaken using a 4-0 nylon tourniquet supported on a piece of silicon so as not to damage the artery. Only under exceptional circumstances is distal occlusion of coronary arteries performed and occlusion devices or intravascular shunts are not used in order to avoid intraluminal damage to the artery.
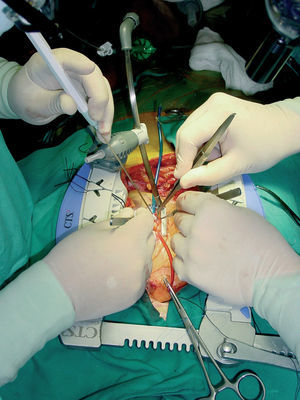
All anastomoses are performed under a stereo microscope (x3.5-x5.5 magnification) with a continuous 8-0 nylon suture (Surgipro, Autosuture, Norwalk, USA) and blood is removed from the arteriotomy with a humidified air blower (Clear View Blower/Mister, Medtronic DLP, Grand Rapids, Michigan, USA) (Figure 11). According to the position of the coronary arteries and the length of the bypass graft we have used both side-to-side (sequential) anastomoses in parallel or perpendicular (diamond configuration) and end-to-side anastomoses, also in parallel or perpendicular.
Figure 11. Complete view of the tools used to perform off-pump coronary artery bypass grafting: Guidant stabilizer, coronary occlusion sutures, and blower.
When each anastomosis is completed a quantitative and qualitative assessment is made using a flowmeter (Transonic System, Ithaca, New York, USA).
Off-Pump Coronary Artery Bypass Grafting: Anticoagulation and Antiplatelet Protocol
Another important characteristic of off-pump circulation is the use of anticoagulants during surgery and their withdrawal following revascularization. Interestingly, Mariani et al50 have demonstrated the presence of procoagulant activity in off-pump coronary surgery that is similar to that which occurs in other major surgery or in percutaneous coronary intervention. It must be taken into account that there is no platelet damage caused by extracorporeal circulation. For us, the essential strategy involves not withdrawing antiplatelet drugs prior to surgery and even administering intravenous antiplatelet drugs at the end of surgery.
CURRENT STATUS
Why Is Conventional On-Pump Coronary Artery Bypass Grafting Not Rapidly Replaced by Off-Pump Surgery?
The microsurgical techniques necessary to perform coronary anastomosis represent one of the fields of most interest to cardiac surgeons. In conventional coronary artery bypass surgery, connection of the patient to extracorporeal circulation is part of the standard procedure and the side effects that can occur are seen as inevitable or attributable to "bad luck," but never to individual error. Performing a coronary anastomosis on a beating heart without the support of cardiopulmonary bypass implies important changes for the surgeon, both technically and psychologically. A surgeon or surgical team that lacks commitment or enthusiasm for learning will find it difficult to satisfactorily undergo "retraining" to perform a new technique. As a group they must be willing to accept some setbacks in the effort to achieve their goal. In an area in which, from the outset, everyone is going to compare off-pump surgery with traditional coronary artery bypass grafting from a severely critical position, it can be very difficult to cope with the necessary learning curve.
In a field such as surgery, which is subject to quite conservative norms, it is both logical and desirable for any change to be analyzed in the finest detail. For these reasons, it is unrealistic to expect the entire cardiac surgery community to welcome the arrival of a new technique in unison. It did not occur with the introduction of the IMA as a coronary artery bypass graft and neither has it occurred with off-pump surgery.
What Has Happened in Off-Pump Surgery During the Last 10 Years?
As mentioned earlier, off-pump surgery has been subject to a process of standardization. This has taken place since the introduction in 1996-1997 of the technology required for correct exposure and stabilization of the coronary artery, suture of the graft, and analysis of its quality.
Thus, the period of genuine interest covers those studies published on patients treated in the last 7 years. Although earlier publications showed clear evidence of limited, incomplete revascularization that yielded poorer results than conventional coronary artery bypass grafting, this was based on a population of patients biased towards the highest risk and with limited technological development.51,52
Current Scientific Evidence: ISMICS Consensus Conference 2004
Of the more than 1200 studies of off-pump coronary artery bypass grafting published and archived in MEDLINE, only around 90 can be considered valuable from the point of view of scientific evidence and, of those, only 37 are randomized trials.
For the analysis, organization, and dissemination to the scientific community of information derived from these studies, a consensus conference was organized in Paris in May 2004 under the auspices of the International Society for Minimally Invasive Cardiac Surgery (ISMICS). The aim of the conference was to use the principles of evidence-based medicine to systematically review and, where appropriate, undertake a metaanalysis of, the evidence from randomized (level A) and nonrandomized (level B) trials comparing off-pump coronary artery bypass grafting with conventional coronary surgery in order to clarify its usefulness in low-risk and high-risk patients.
The conference was planned and structured according to the American College of Cardiology and American Heart Association (ACC/AHA) standards for the preparation of clinical practice guidelines.
Following information retrieval from 7 different databases, a systematic review and metaanalysis of 37 randomized trials comparing the 2 techniques in patients of varying risk was performed. In addition, 2 metaanalyses of nonrandomized studies in patients of varying risk were identified. No systematic reviews, randomized trials, or metaanalyses were identified in high-risk patients. Consequently, a metaanalysis was undertaken to address this question.
The primary objective was to analyze all-cause mortality at 30 days and 1 year for each of the 2 techniques. As secondary objectives, the following were assessed: the incidence of postoperative stroke, cognitive dysfunction, acute myocardial infarction, recurrent angina, repeat intervention, requirement for inotropic drugs, need for intraaortic balloon pump, atrial fibrillation, renal failure, mediastinitis, respiratory infection, repeat intervention for bleeding, and requirement for transfusion, along with length of stay in intensive care, hospital stay, cost, and quality of life.
While awaiting the definitive publication of the conclusions and recommendations of the ISMICS Consensus Conference 2004 in the next few months, it has been indicated that there is a consensus in the following areas (Anno Diegeler, personal evaluation; available at www.cts.org): off-pump coronary artery bypass grafting is safe and effective and there is no significant difference in mortality compared with conventional coronary surgery in studies performed on mixed-risk patient groups. Complete revascularization can be achieved with both techniques,53-55 without significant differences in studies performed on mixed-risk patient groups. There are no significant differences between the 2 techniques in terms of early clinical56 or angiographic53-55 results, or the results at 6 to 12 months.57-60 In areas such as cognitive deterioration,61-64 use of blood products,65,66 myocardial ischemia, and cost, the results favor off-pump surgery.67-69 Nonrandomized, risk-adjusted, retrospective studies undertaken using large databases show a reduction of in-hospital mortality in high-risk patients who undergo off-pump surgery.70-76
Analysis of studies with different results to those indicated above leads to a clear conclusion: off-pump coronary artery bypass grafting can be performed with good and predictable results by experienced surgeons. The fact that this is not the case with inexperienced surgeons emphasizes the importance of specific training programs in the use of this new technique.77
In May 2005, the American Heart Association published a "scientific statement" on comparisons between OPCABG and conventional coronary artery bypass grafting.78 Their conclusions essentially coincide with those of the ISMICS Consensus Conference 2004. In essence, they attribute clinical advantages to OPCABG, whereas conventional CABG is suggested to offer the advantage of technical simplicity. In our experience, while the technical difficulties can be overcome with adequate training, the clinical advantages can be neither substituted nor undervalued.
Results of the First 1000 Patients Treated at Juan Canalejo University Hospital Complex, Spain
The use of off-pump surgery in complete arterial revascularization has increased exponentially in our hospital and represents more than 96% of all isolated coronary artery bypass grafting performed in recent years. Here we summarize the results of the first 1000 patients who underwent this type of surgery.
A total of 1000 patients underwent off-pump revascularization surgery between April 1998 and January 2004; 828 of the patients were men (82.8%) and the mean (SD) age was 67 (9.5) years (range, 23-90 years). Unstable angina was presented by 66% of patients, diabetes by 29.3%, and peripheral arteriopathy by 14.7%. Lesions of the left main coronary artery were found in 20% of patients, 57% had triple vessel disease, and 18% had 2-vessel disease. Mean ventricular function was 60% (13%) with a range of 15% to 88%. Both IMAs were dissected free of pedicle and anastomosed in a Y or T graft configuration to reach the different territories. Graft patency was assessed by intraoperative Doppler.
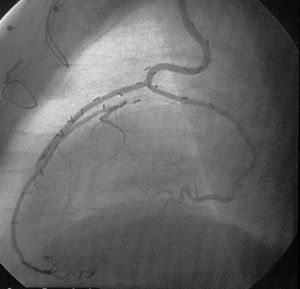
A total of 2740 distal anastomoses were performed, with a mean of 2.74 (range, 1-5) per patient, 62% of patients receiving 3 or more grafts. In terms of surgical morbidity, 66 patients (6.6%) presented postoperative atrial fibrillation; 32 (3.2%), perioperative infarction; 12 (1.2%), mediastinitis; 14 (1.4%), repeat intervention for bleeding; and 4 (0.4%), permanent stroke. In-hospital mortality was 3.5% (35 patients). In the year 2000, a randomized study of graft patency was performed in patients who had undergone surgery at least 6 months earlier and 98% patency was observed (Figure 12).79 With a maximum of 6 years of follow-up, the incidence of repeat revascularization is 1.5%.
Figure 12. Coronary angiography of one of our patients revascularized using off-pump surgery. Left internal mammary artery (IMA) graft to the anterior descending artery and right IMA as a free graft in a T configuration from the left IMA to the first marginal branch.
THE FUTURE OF OFF-PUMP CORONARY ARTERY BYPASS GRAFTING
In future years, new techniques for coronary angioplasty will have an even greater impact on the clinical and anatomic profile of patients in whom coronary artery bypass grafting is indicated. The demands placed on surgery will be even greater if it is to offer satisfactory results. In this context and with current evidence, it is logical to suppose that the advantages provided by off-pump surgery will gain weight in the future--but the "retraining" must begin now.
More importantly, the arrival of new generations of young cardiac surgeons trained in these new techniques from the outset may result in an exponential increase in their improvement and use. National cardiac surgery societies, industry, and senior surgeons are obliged to facilitate this transformation through the provision of training.
CONCLUSIONS
1. Off-pump coronary artery bypass grafting is performed in hundreds of hospitals throughout the world. It currently represents 20% to 30% of the total. More than 1200 studies have been published in international journals.
2. Patients are selected according to the experience of the surgeon. It is possible to perform complete arterial revascularization without patient selection.
3. The technique reduces some aspects of morbidity and the consumption of health-care resources in low-risk patients, and reduces mortality and morbidity in those patients who are at high risk.
4. Off-pump coronary artery bypass grafting is here to stay.
Section Sponsored by Laboratorio Dr Esteve
Correspondence: Dr. J. Cuenca.
Servicio de Cirugía Cardíaca. Hospital Juan Canalejo.
As Xubias, 64. 15006 A Coruña. España.
E-mail: josecuenca@cardiocrunia.com