Keywords
INTRODUCTION
Therapeutic, pharmacological or surgical interventions in any disease should aim to improve prognosis in terms of mortality, symptoms or quality of life. Coronary revascularization, whether by bypass surgery or percutaneous coronary intervention, should therefore only be used when the evidence available suggests that patients will benefit in one of these 3 ways. The patient should therefore not only undergo a careful anatomical examination but should also always be submitted to clinical and functional assessments.
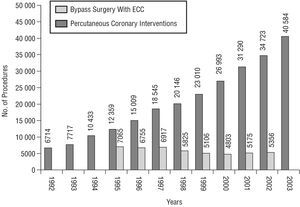
Coronary revascularization as a therapeutic strategy has been widely accepted for many years, though the procedures have been constantly developed and expanded. Vineberg and Millar1 made the first attempt to surgically improve perfusion in an ischemic area in 1951. Their procedure consisted of grafting the internal mammary artery directly into the myocardium. Coronary surgery in its current form was first done by Kolesov and Potashov,2 who performed a coronary artery bypass graft with a mammary artery in 1964, and Favaloro,3 who carried out the first saphenous vein aortocoronary bypass in 1967. Percutaneous coronary intervention (PCI) is a more recent technique, though it is already more than a quarter of a century old. Grüntzig et al4 did the first percutaneous transluminal coronary angioplasty (PTCA) in 1977. Since then, this revascularization technique has expanded rapidly and continues to be developed today. According to the latest figures from the registries of the Spanish Society of Cardiovascular Surgery5 and of the Working Group on Cardiac Catheterization and Interventional Cardiology of the Spanish Society of Cardiology,6 patients in Spain underwent 8617 coronary bypass operations with or without extracorporal circulation in 2002 and 40 584 PCI in 2003. As shown in Figure 1, the number of PCI continues to rise at a rate of around 15% a year, whereas the number of coronary surgical procedures has leveled off after a slight drop at the end of the nineties. Greater availability, better outcomes thanks to technical advances and a greater experience and knowledge of the clinical and pathophysiological mechanisms of coronary artery disease can explain these trends. As a result, the number of patient groups shown to benefit from coronary revascularization and in whom such an intervention is possible has increased. We currently have a wealth of information on the results of different revascularization techniques, both overall and for different subgroups of patients of special interest because of their characteristics or complexity. This should improve the selection of patients indicated for revascularization.
Figure 1. Change in the number of percutaneous coronary interventions and coronary bypass operations with ECC done in Spain according to data from the Registry of the Working Group on Cardiac Catheterization and Interventional Cardiology of the Spanish Society of Cardiology6 and the Spanish Society of Cardiovascular Surgery.5 ECC indicates extracorporeal circulation.
The revascularization process comprises 2 parts: indication and selection of type of revascularization, and the intervention itself. Both should be rigorously implemented to ensure that the patient benefits from the intervention and it is essential that cardiologists participate in the first part, that is, the detection and selection of patients who may benefit from a revascularization process. The final decision should not be based solely on anatomical findings from coronary angiography but also on an assessment of clinical factors, information on how coronary stenosis affects cardiac function, ventricular function and the outcomes in the services themselves where the intervention will be done. The clinical assessment is a decisive step in the final outcome of the revascularization. In this article, we review the indications with their corresponding clinical considerations and the choice of type of revascularization in patients with stable ischemic heart disease and non-ST segment elevation acute coronary syndrome (NSTE-ACS).
CLINICAL FACTORS IN THE INDICATION OF REVASCULARIZATION: INDICATORS AND PROGNOSTIC ALGORITHMS
The indication of a revascularization procedure, whether bypass surgery or PCI, should take into account a series of limitations and risks in each patient, and should only be undertaken when it is anticipated that life expectancy will be extended or quality of life improved. The specialist should therefore evaluate the symptoms of each patient and how these might be affected by revascularization. The search for prognostic markers and the creation of decision algorithms will help identify populations at high risk, that is, those that will benefit most from a revascularization procedure that aims to improve prognosis. The impact of some clinical factors (diabetes, age, and renal impairment) is so important in the decision making process that these factors will be considered in separate sections.
Stable Ischemic Heart Disease
The group of patients with stable ischemic heart disease is broad and includes those with stable angina who have never been assessed for possible revascularization, asymptomatic patients with known ischemic heart disease (after surgery, PCI or ACS), and patients whose angina cannot be treated by revascularization (refractory angina). The indication to undergo revascularization based on symptoms is according to the perception of its severity of symptoms according to both the specialists and the patients (severity is usually graded according to the classification of the Canadian Cardiovascular Society). Prognostic markers have been identified in patients with stable angina, and these need to be assessed when deciding whether a revascularization procedure is indicated. These markers are summarized below.
Heart Failure or Evidence of Left Ventricular Dysfunction
Prior history of heart failure7,8 or evidence of left ventricular dysfunction8-10 is a clear marker of poor prognosis. Studies have shown that less than 35% of patients with chronic ischemic heart disease are associated with a particularly high mortality rate--greater than 3% per year. The greater probability of complications does not depend on the frequency and severity of angina or the number of diseased vessels, although prognosis is worse when these factors are associated. Thus, less than 60% of patients with 3 diseased vessels and a low ejection fraction remain free from infarction after 2 years.
General Clinical Markers
Clinical characteristics other than diabetes mellitus or renal impairment (both considered separately) are strong indicators of the clinical course of patients. These markers include:
- Advanced age: mortality and rate of nonfatal ischemic events increase with age, as shown in widely cited studies such as the Framingham heart study11 and other more recent ones.12
- Prior myocardial infarction: this is a marker associated with left ventricular dysfunction and also with a higher mortality or rate of ischemic complications.9,13
- Frequency and severity of angina: this is also a prognostic marker in all groups, regardless of ventricular function and extent of the disease. For example, in patients with more than 3 diseased vessels and normal left ventricular function, event-free survival after 2 years is around 90% when the patient has infrequent mild angina, and less than 70% in patients with frequent severe angina.9
- Abnormalities in the resting electrocardiogram with indications of prior infarction, left bundle branch block or resting repolarization abnormalities are associated with a worse prognosis. Patients with resting ST-segment depression, electrocardiographic findings indicative of prior infarction or repolarization abnormalities have a higher mortality and a greater probability of suffering myocardial infarction.13,14
Findings of Tests to Assess Cardiac Function in Coronary Artery Disease and the Detection of Viable Myocardium in Regions With Abnormal Wall Motion
In order to assess the need for revascularization in patients with stable ischemic heart disease, tests to assess the effect of coronary artery disease on cardiac function are essential in most cases. Often, it is also necessary to determine myocardial viability in akinetic areas. The most widely used assessment is conventional exercise testing but specialists are increasingly using the findings from imaging techniques to guide their decisions. The next section summarizes the use of such techniques.
Coronary Anatomy: Angiographic Findings
A wealth of prognostic information can be obtained from the coronary anatomy determined by coronary angiography. This technique is indicated in most patients, and the findings from tests in which ischemia is induced or the assessment of predictive clinical factors can indicate whether the prognosis or symptoms of a patient will benefit from a revascularization procedure. Knowledge of the coronary anatomy will confirm whether revascularization is necessary, provide information on whether the procedure is technically viable and, most importantly, help choose the type of revascularization. The number of diseased vessels is an important predictor of adverse events, particularly in association with left ventricular dysfunction. Survival after 12 years in patients with 3 diseased vessels and normal ventricular function was almost 50%, but decreased to less than 20% when associated with an ejection fraction below 35%.10 The angiographic findings associated with a poor outcome are summarized in Table 1.
Several grading systems for patients with coronary artery disease have been developed.9,10,15-18 These are based on clinical characteristics and results from stress tests. However, the dynamic nature of different diagnostic techniques and the continuous therapeutic advances complicate the application of these indices. The specialist will usually make his final decision taking into account an assessment of the severity of the angina, associated risk factors, response to pharmacological treatment, age, sex, ventricular function, risk markers in tests of induced ischemia, site of the coronary lesions, and their distal beds. Accessibility and the outcomes of different types of revascularization in the hospital itself are also important considerations.
Non-ST Segment Elevation Acute Coronary Syndrome
The therapeutic strategy for treating NSTE-ACS has changed considerably in recent years for 3 reasons. First, the course of ACS is better defined and new biochemical markers have been developed, allowed grading algorithms and systems to be constructed that provide information on risk and therefore on prognosis. Second, the use of potent antiplatelet agents (thienopyridines and glycoprotein IIb/IIIa inhibitors) has improved the clinical course of patients with ACS. Finally, patients with high-risk NSTE-ACS have been shown to benefit clinically from an early interventional strategy consisting of coronary angiography and revascularization.19-22 Thus, identification of this subgroup of patients has become of utmost importance. Furthermore, patients with NSTE-ACS must be stratified early because more than half the complications in such patients occur in the first days, and there is no definite cutoff point. Correct assessment and treatment in the early phases should therefore lead to a decrease in mortality and nonfatal ischemic complications in such patients.19 Grading systems have thus been developed so that patients can be classified quickly and those at high risk identified. The most widely used systems are the ones developed by the TIMI investigator group (TIMI score)23 and the stratification scales of the Spanish24 and European25 Societies of Cardiology.
TIMI Risk Score
To determine the TIMI risk score, 7 prognostic variables were selected for the population assigned to unfractionated heparin in the TIMI 11B trial.23 The variables selected are listed in Table 2. The score is calculated by summing the number of variables that are true for each patient.
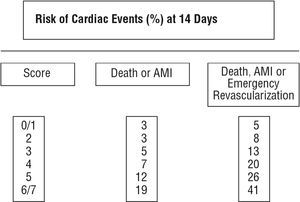
As shown in Figure 2, the risk of complications (overall mortality, myocardial infarction, or recurrent ischemia requiring revascularization after 2 weeks) is directly proportional to the score. This grading system was validated retrospectively for the group assigned to enoxaparin in the TIMI 11B study and prospectively in the ESSENCE study. The findings of both studies were consistent.
Figure 2. Risk of events after 14 days in patients with non-ST segment elevation acute coronary syndrome according to TIMI score.23 AMI indicates acute myocardial infarction.
Classification System of the Working Group on Ischemic Heart Disease of the Spanish Society of Cardiology and the Coronary Working Group of the European Society of Cardiology
The guidelines for clinical practice issued by the Spanish Society of Cardiology define 3 groups of risk (high, intermediate, and low), referring to the risk of death, myocardial infarction, refractory ischemia, or ventricular arrhythmias in the following 30 days. The characteristics that define each group are shown in Table 3. On the other hand, the Guidelines of the European Society of Cardiology divide patients with NSTE-ACS into 2 groups: high and low risk. Patients at high risk are those that meet at least one of the following criteria:
- Recurrent ischemia defined as recurrent angina or presence of dynamic ST segment changes (in particular, ST segment depression, or transient elevation).
- Postinfarction angina.
- Elevated troponin.
- Hemodynamic instability during the observation period.
- Severe ventricular arrhythmias.
- Diabetes mellitus.
- Electrocardiographic pattern that prevents correct assessment of changes in the ST segment.
Patient stratification must be associated with a therapeutic strategy that will be adjudged to improve quality of life or prognosis on the basis of available evidence. Thus, identification of high risk patients using any of these risk evaluation systems will not only indicate an early revascularization strategy but will also influence the choice of antithrombotic therapy and antiplatelet treatment.
COMPARISON OF THE DIFFERENT TECHNIQUES FOR DETECTION AND QUANTIFICATION OF ISCHEMIA AND VIABILITY: THEORY AND PRACTICE
In patients with stable ischemic heart disease or NSTE-ACS with unknown coronary artery anatomy, that is, those who have not been subject to an early interventional strategy, a technique should be applied to quantify the severity of the ischemia to identify those patients who may benefit from revascularization. Furthermore, even in some patients with known coronary artery anatomy, the viability of akinetic areas may need to be determined in order to assess the potential benefit of revascularization. Currently, many techniques are availa ble for quantifying ischemia (estimating the effect on cardiac function of coronary artery disease) and for detecting and quantifying the existence of myocardial viability.26
Techniques for Estimating the Effect on Cardiac Function of Coronary Artery Disease
Stress Tests
Specialists have essentially 4 techniques at their disposal for estimating the functional importance of coronary artery disease by stress tests, namely: conventional exercise testing, stress echocardiography, nuclear exercise stress testing, and dobutamine-stress magnetic resonance imaging (MRI).
Conventional exercise testing is of proven usefulness for both diagnosis and prognostic evaluation of coronary artery disease, measurement of functional capacity and treatment response. The sensitivity and specificity of the technique are around 67% and 72%, respectively, and depend on prevalence of the disease in the study population and the severity of the coronary artery disease.27 Drug-induced or exercise stress echocardiography is more sensitive and specific than exercise testing for detecting impaired overall or regional contractile function when present alongside abnormalities in the electrocardiogram, in response to exercise- or drug-induced ischemia. Sensitivity decreases with prior pharmacological treatment and contractile abnormalities at rest. Currently, sensitivity is taken to be between 74% and 97% and the specificity to be between 70% and 100%.27,28 Nuclear exercise testing has a similar predictive capacity to that of stress echocardiography. For each of these techniques, criteria associated with poor prognosis have been established and their presence demands revascularization to be considered (Table 4). Finally, dobutamine MRI offers a sensitivity of 86% to 90% and a specificity of 86% to 95%.28,29
These stress techniques for detection of ischemia are subject to advantages and drawbacks that determine their usefulness in a given hospital. The conventional exercise test is the most widely used because it is also the most widely available. The limitations of this technique for detecting coronary artery disease in certain patients (those with resting electrocardiographic abnormalities, preexcitation syndrome, conduction disorders, women) have accelerated the development of other imaging techniques. Stress echocardiography is sensitive and specific, but is also limited (some patients have a poor echocardiographic window, the evaluation of regional contractility is subjective, the endocardium may not be optimally visualized, or necrotic or ischemic tissue may be unevenly distributed). Its negative predictive value is lower than that of other techniques27 but its wide availability, low cost, the possibility of bedside tests with immediate results and the lack of ionizing radiation make it the technique of choice in most hospitals with experience of such patients. Nuclear techniques, on the other hand, are less widely available and require radioactive material, but they have the advantage over echocardiography that the findings are less dependent on the observer. Magnetic resonance imaging has obvious advantages, namely: reproducible images of excellent quality can be taken for all patients that are independent of subjective judgments of the clinician; the sectioning can be reproduced at each stage of the protocol; the surfaces of the chamber and the epicardium can be readily identified and the structures differentiated from blood; and the thickness and thickening of the wall can be accurately measured.26 The limited availability of this technique, related not only to whether the hospital has MRI facilities, but also to the need to control the timing and necessity of a close coordination between 2 hospital services (cardiology and radiology) and the high cost hinder a more widespread use of the technique in such patients.
Myocardial Perfusion Studies
Decreased myocardial perfusion (initially subendocardial) is an indicator of ischemia. The most widely used method in clinical practice for measuring such decreases is single photon emission computed tomography (SPECT), a technique with a sensitivity of 83% to 95% and a specificity of 53% to 95%, but with low spacial resolution.30 In contrast, the high spacial resolution afforded by MRI allows subendocardial perfusion deficiencies to be seen in studies of first pass kinetics of gadolinium after intravenous administration. The myocardial areas with abnormal perfusion appear as dark areas during maximum hyperemia (because the arrival of contrast is delayed), but not at rest. Abnormal perfusion is classed as permanent or reversible. Recent studies have achieved a sensitivity of 91% and a specificity of 94% for the detection of coronary artery disease. According to the number of affected vessels, some authors obtain a sensitivity of 84% for single vessel disease, 90% for 2 diseased vessels, and 93% for 3 diseased vessels.26
Techniques for Detection and Quantification of Viable Myocardium
It is important to be able to identify viable myocardium because revascularization in patients with a large area of dysfunctional viable myocardium has a positive impact on morbidity and mortality of patients with a high incidence of severe coronary events.31,32 Characteristically, viable myocardium conserves both the thickness of the ventricular wall and other features such as contractile reserve, membrane integrity, metabolism, mitochondrial integrity and blood perfusion. Diagnostic techniques that study myocardial viability are based on the detection of some or several of these markers of viability. The ideal diagnostic technique would have sufficient spatial resolution to define the extent of viable myocardium within a given ventricular region. Several techniques are available for studying myocardial viability, and these are briefly considered below.
Techniques That Assess Myocardial Viability by Evaluating Contractile Reserve
Stress echocardiography is the most representative technique for evaluating viability through analysis of contractile reserve. Biphasic response is characteristic of viable myocardium and predicts the recovery of ventricular function after revascularization.33,34 The technique is subject to the same limitations as when used to detect ischemia. In addition, significant coronary stenosis may cause ischemia with lower oxygen uptake at low doses of dobutamine. If this technique is compared with SPECT or positive emission tomography (PET), dobutamine stress echocardiography is more specific (81% compared to 47% to 73% for the other techniques) and less sensitive (84% compared to 83% to 90% for the other techniques) for diagnosis of viability.
Cardiac Magnetic Resonance Imaging
Cardiac MRI with gadolinium contrast is the most accurate and most simple detection technique to perform33 and the one that provides greatest spacial resolution. Viability is determined by detecting late enhancement. Late enhancement is not detected in ischemic areas, but abnormalities in myocardial thickening can show up because of the existence of stunned or hibernating myocardium. The high spacial resolution inherent in cardiac MRI can reveal the extent of viability within the ventricular wall, distinguishing between abnormal subendocardial and subepicardial tissue and identifying abnormalities that span the entire wall. Currently, many studies are available showing that the recovery of contractility is directly related to the percentage of transmural viable myocardium. The advantages of cardiac MRI are related to its high precision, its simplicity (no stress is required), the use of a safe contrast, and its reproducibility.
Nuclear Techniques
Late-uptake of thallium 201 is measured. The most preferred technique in nuclear cardiology laboratories at present is gated-SPECT. Simultaneous evaluation of the myocardial perfusion and overall and regional contractility is possible by acquisition of isotopic images of myocardial perfusion synchronized with the electrocardiogram and gated-SPECT. The performance of this technique for evaluating the presence of viability has been studied by determining the contractile reserve during dobutamine perfusion at 10 µg/kg/min, giving a sensitivity of 96% and a specificity of 78%.
Other Techniques That Assess Myocardial Viability
Myocardial viability can be assessed by other techniques, but they are less widely used in clinical practice. These techniques include a combined assessment of myocardial microperfusion and membrane integrity (radioisotopes or cardiac MRI); combined assessment of coronary microperfusion and contractility (perfusion echocardiography), and evaluation of cell metabolism. Positron emission tomography is the most relevant technique in this group and has been considered as the gold standard until the development of cardiac MRI. Its predictive value for identifying contractility after revascularization is between 80% and 87%.31 The biggest disadvantage of PET is its high cost and low availability. The other technique that can be used to assess viability by metabolic analysis is cardiac MRI, but this approach is currently only used in clinical investigation.
Clinical Features of the Different Techniques for Detection of Ischemia and Viability in the Revascularization Process
In patients with stable ischemic heart disease, or in those with unstable but stabilized ischemic heart disease, tests are necessary to detect and quantify ischemia to assess the need for revascularization. For most hospitals, conventional exercise testing is the first step because it is easy to do and widely available. As discussed earlier, this test is, however, subject to limitations in some subgroups of patients (those with abnormal resting electrocardiogram, those on certain drugs, women, or those with motor deficit). Therefore, all cardiology services need to have other stress tests available able to detect abnormalities in myocardial perfusion (coronary scintillography) or ventricular function (stress echocardiography) both at rest and during dynamic or pharmacological overload. Their sensitivities and specificities overlap, so the choice of one or the other will depend on the experience of the hospital and the availability of the technique. Stress echocardiography or nuclear studies would be indicated when exercise testing is limited, the clinician needs to know the site and extent of ischemia or assess the effect on cardiac function of a coronary lesion, or the clinical signs and symptoms do not agree with the result of the exercise testing. Cardiac MRI, which has been shown to be a precise reproducible technique that does not depend on subjective impressions of the patient or on the clinician who interprets the scans, is restricted in most hospitals to the most complex cases with inconsistent or inconclusive findings in other tests. Nevertheless, technical advances may expand the use of cardiac MRI for assessment of revascularization in patients with ischemic heart disease in the future.
Two questions need to be considered with regard to viability studies in akinetic regions, namely, when is such study necessary and what technique should be applied. The extent of viable myocardium in a patient awaiting revascularization can provide information on the potential improvement in ventricular function after revascularization and, therefore, on the long-term prognosis as well as on the improvement in functional grade. Revascularization is indicated in patients with extensive coronary artery disease and severe ventricular dysfunction with evidence of ischemia, as this is associated with better long-term prognosis. But in the subgroup with a high surgical risk, the amount of viable myocardium, and therefore the amount of myocardium that can be recovered, should be carefully assessed to determine the risk-benefit ratio. In some patients, incomplete percutaneous coronary revascularization may even be an alternative to a bypass operation if we can rule out viability in areas that will not be revascularized. A recent metaanalysis35 assessed the prognostic benefit associated with revascularization in patients with viable myocardium and ventricular dysfunction. Mortality was higher among patients with viable myocardium treated medically than those without viable myocardium treated medically. Furthermore, among patients treated by revascularization, those with viable myocardium had a lower annual mortality rate, and an inverse relationship with ejection fraction was found, that is, the lower the ejection fraction, the greater the benefit of revascularization. Another subgroup of patients for whom determination of viability was of potential interest comprises those with acute myocardial infarction. Support for revascularization of the infarct-related artery may be obtained from measurement of viable myocardium in the infarct area, but there is no evidence with regard to improvement of long-term mortality.
Cardiac MRI is the technique of choice for studying myocardial viability at present due to its simplicity and reliability. As discussed earlier, the main limitation is its lack of availability; therefore all cardiology services should be familiar with echocardiographic or nuclear techniques (depending on the experience and resources of each hospital) to evaluate myocardial viability in patients for whom such a study is indicated.
CLINICAL FACTORS IN THE INDICATION OF REVASCULARIZATION IN SPECIAL PATIENT SUBGROUPS
There are 4 subgroups of patients in whom revascularization requires special attention. These subgroups are elderly patients, diabetic patients, patients with renal impairment, and women.
Revascularization in Women
The outcomes of revascularization differ for men and women. For percutaneous revascularization, pooled outcomes are unfavorable for women, who have higher rates of hospital mortality, even with the advent of stenting and the use of glycoprotein IIb/IIIa receptors. The reasons for these differences are not completely clear but a number of factors are thought responsible, for example, women undergoing these procedures may be older and have high blood pressure, left ventricular hypertrophy, diabetes mellitus, and coronary arteries with a smaller diameter.36 The situation is similar for bypass surgery, with higher hospital mortality among women. This difference is particularly large for female diabetics who happen to represent a particularly important subgroup of women with coronary artery disease. Most surprising of all is the striking difference in hospital mortality between young men and women, a difference that becomes less marked with age. A review of the findings from medium- and long-term (1 to 5 years) follow up of patients who have undergone percutaneous revascularization and bypass surgery shows that the initial differences between men and women disappears.37 To summarize, and in view of all the evidence available, the sex of a patient should not be taken into account when deciding whether to perform a revascularization procedure.
Revascularization in Elderly Patients
Elderly patients have a number of characteristics that complicate the diagnosis and management of coronary artery disease with respect to the general population. Noninvasive diagnosis is more difficult because, on one hand, resting electrocardiograms tend to show more abnormalities and, on the other, the elderly patient is unable to carry out exercise. Diagnostic coronary angiography, however, hardly carries more risk than in younger patients, and so this technique is widely used among elderly patients.
The prognosis of coronary artery disease deteriorates with age. For those with NSTE-ACS, the biomedical literature supports an invasive strategy compared to conservative strategy, particularly in patients at high risk. In clinical trials in which these 2 strategies were compared--TIMI IIIB,38 FRISC-II,20 and TACTICS21--the benefit of the invasive strategy was greater in the subgroup of patients over 65 years. In patients with stable ischemic heart disease, recommendations about indications of revascularization are the same for patients with stable ischemic heart disease, regardless of age, though it is obviously necessary to assess the (increased) risk-benefit ratio, particularly with respect to quality of life and especially for patients over 80 years old.
With regard to angioplasty, one of the main risk factors for complications is age greater than 75 years. However, with the introduction of stents into clinical practice, the procedural success rate and short-term outcomes are similar to those of younger patients. Therefore, the clinical guidelines do not have a special category for elderly patients. Nevertheless, the greater prevalence of concurrent diseases should be remembered when the need for angioplasty is considered in these patients.39
For coronary bypass surgery, the incidence of complications in elderly patients is higher than in the remaining population, partly because elderly patients generally have more advanced coronary artery disease and partly because these patients have more concurrent diseases. The surgical risk is directly related to age--the mortality associated with coronary bypass surgery is calculated to be around 1.65% for patients aged between 50 years and 60 years, and increases to 8.31% for those aged over 80 years. Nevertheless, a re asonably high proportion of these patients obtain a substantial improvement in quality of life after the operation. Advanced age per se should not, in principle, contraindicate coronary bypass surgery if the clinician believes the long-term benefits outweigh the risks of the operation.40
Revascularization in Diabetic Patients
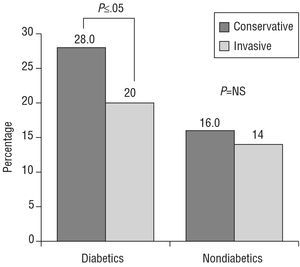
Coronary artery disease is highly prevalent among diabetic patients. In fact, diabetes mellitus is considered an equivalent of cardiovascular disease. However, diabetes is associated not only with a high rate of coronary artery disease but also with a worse prognosis.41 The indications of revascularization in diabetic patients with stable ischemic heart disease are essentially the same as for the general population. Revascularization procedures are more beneficial than medical treatment despite the higher mortality associated with revascularization in diabetic patients compared to nondiabetic patients, as shown in the CASS study.42 An aggressive invasive strategy has been shown to be beneficial compared to conservative management guided by ischemia in patients with NSTE-ACS.41 A decrease in mortality and rate of myocardial infarction were observed in the FRISC II20 and TACTICS21 studies with invasive strategies, and these benefits were maintained in the group of patients with diabetes. In fact, the benefit for patients assigned to the invasive group of the TACTICS study was due essentially to the benefit among diabetic patients, as shown in Figure 3. Of the 2220 patients included, 28% had diabetes, and the incidence of death, reinfarction, or readmission due to ACS decreased by 28% among such patients who were assigned to the interventional strategy (compared to a reduction of 20% in patients not assigned to such therapy; P<.05). The decrease was not significant in nondiabetic patients (16.4% vs 14.2%).
Figure 3. Incidence of the primary endpoint (mortality, percentage with nonfatal myocardial infarction, or rehospitalization) at 6 months in diabetic and nondiabetic patients for invasive treatment versus conservative treatment of acute coronary syndrome in the TACTICS-TIMI-18 study.21
Balloon angioplasty in diabetic patients is associated with worse medium- and long-term outcomes than in nondiabetic patients because of a higher incidence of restenosis and a faster progression of the coronary artery disease in untreated segments.43,44 The initial and long-term outcomes have improved and the incidence of restenosis has decreased as a result of the increased use of stents, but diabetic patients still fair worse than nondiabetics.41 Coronary bypass surgery, like angioplasty is associated with greater mortality in diabetic compared to nondiabetic patients. Nevertheless, the survival benefit is greater than with medical treatment. If we compare the 2 revascularization techniques, the results of the BARI study45,46 showed that diabetic patients with more than 1 diseased artery had a significantly better survival after bypass surgery than after PCI provided that the bypass was done with at least 1 mammary artery graft. The findings of this study are subject to a number of limitations, particularly with regard to the technique, as neither stents nor glycoprotein IIb/IIIa inhibitors were used, but subsequent studies such as the ARTS47 drew similar conclusions.
Therefore, when revascularization is indicated, the best approach seems to be to opt for angioplasty in diabetic patients with single-vessel disease and to consider bypass surgery as the first choice in patients with more than one diseased vessel. The decision, however, should be individualized in each case, taking into account factors such as the size of the vessels and concurrent diseases of the patient before surgery. The use of drug-eluting stents that inhibit intimal hyperplasia may substantially reduce restenosis and this may shift the balance in the decision of what treatment to use in diabetic patients with multivessel disease in the future.
Revascularization in Patients With Renal Impairment
Chronic renal insufficiency (CRI), regardless of severity, worsens the prognosis of coronary artery disease. Moreover, the incidence of ischemic heart disease is higher in patients with CRI than in the general population. Thus, the prevalence of coronary artery disease in dialysis patients is 40% and cardiovascular mortality is 9%.48
Clinical assessment is more complex in patients with CRI because atypical symptoms appear more often, the electrocardiogram is less specific (ST and T-wave abnormalities) because of electrolyte imbalances, particularly in patients who undergo dialysis, and the sensitivity of the nuclear stress test is low. Dobutamine stress echocardiography is the most reliable technique for detecting ischemia, with a sensitivity that ranges between 75% and 95% and a specificity that ranges between 76% and 86%.49 Often, the clinician must resort to invasive diagnosis by means of coronary angiography, but the contrast may induce nephropathy that can lead to a deterioration in renal function which, although generally reversible, can be severe enough that some patients may require dialysis or be forced onto the dialysis program earlier.
Little information is available on PCI in patients with CRI. Balloon PCI has an angiographic success rate of 56% to 96%, but a high rate of restenosis (60%-81%).50 The use of stents has improved the angiographic outcomes (>90%) and lowered the rate of restenosis (31%-36%).51 The new drug-eluting stents may improve outcomes, but evidence has yet to confirm this improvement.52 Coronary bypass surgery leads to an increase in postoperative disease and mortality (between 7% and 10%) in patients undergoing dialysis--three times higher than in patients without CRI--and the mortality at 5 years is estimated to be 48% compared to 15% in patients who conserve their renal function.53 The BARI (Bypass Angioplasty Revascularization Investigation) study showed an increase in all-cause mortality, as well as in cardiac mortality, and an increase in readmission to hospital in patients with CRI who underwent PCI or coronary bypass surgery.54 Studies have even shown the same mortality for bypass surgery in patients with mild or moderate renal impairment compared to those in hemodialysis programs.
Studies that compare PCI with coronary bypass surgery in patients on dialysis are retrospective and nonrandomized. Survival and symptoms are better for coronary bypass surgery though greater perioperative mortality is seen. Preliminary reports on a large prospective study that compared PCI with stenting to bypass surgery in patients with multivessel disease suggest similar results in both groups.55 However, the multivariate analysis of a recent prospective observational study showed that the outcome for bypass surgery was better than that for PCI in multivessel coronary artery disease and in the presence of multiple risk factors (age, diabetes, respiratory diseases, peripheral artery disease, left main coronary artery disease, or diffuse coronary artery disease).56
For ACS, the clinical signs and symptoms, diagnosis and treatment are similar to those of patients without CRI. Troponin T and troponin I are usually elevated, and so they loose predictive capacity.57 A nonrandomized study in patients with CRI with creatinine clearance <60 mL/min and ACS showed that at long-term follow up (60 months) the improvement in survival was greater with PCI than with coronary bypass surgery.58 It is interesting to highlight that this study shows that aggressive therapy (PCI or coronary bypass surgery) is better than medical treatment in patients with ACS.
REVASCULARIZATION IN THE THERAPEUTIC STRATEGY FOR STABLE ANGINA AND NSTE-ACS
Stable Ischemic Heart Disease
Outcomes of Revascularization in Stable Ischemic Heart Disease
Revascularization in stable angina and NSTE-ACS aims to improve either symptoms or prognosis. With regard to the improvement in symptoms, bypass surgery has been shown to be effective, both in clinical trials59 and large observational studies.60-62 In the CASS study, 66%, 63%, and 47% of patients randomized to bypass surgery were asymptomatic after 1, 5, and 10 years, respectively, compared to 30%, 38%, and 45%, respectively, of patients assigned to medical treatment.63 Percutaneous coronary interventions have also been shown to be more effective than medical treatment for controlling symptoms. Few randomized studies have been published comparing angioplasty with medical treatment in patients with 1 or 2 diseased vessels (ACME,64,65 RITA-2,66 AVERT,67 and ACIP68,69). In conclusion, these studies demonstrate that coronary angioplasty is better than medical treatment at controlling symptoms and improving functional capacity in patients with single-vessel or 2-vessel disease, without increasing the long-term need for further revascularization procedures. The effect of angioplasty on mortality is controversial, and so it should be reserved for highly symptomatic patients or those with substantial ischemia. However, these studies have an important limitation when interpreting their findings in the current setting, namely, the PCI techniques used in these studies, which correspond to those used before the advent of new devices and antiplatelet agents, and bear little resemblance to those used today.
The ability of bypass surgery to improve prognosis was shown for some patient subgroups (those at greatest risk and with worst natural course) in 3 studies--VACS,13 ECSS59, and CASS63--which have become widely cited. The VACS study showed greater survival for patients with left main coronary artery disease or triple vessel disease with left ventricular dysfunction, essentially in the first 7 years after the intervention. The CASS study showed improvement in survival in patients with 3 diseased vessels and low ejection fraction (79% vs 61% after 10 years). The ECSS was the only one of the 3 studies that showed improved prognosis in the overall group treated with bypass surgery. The study also identified new groups of patients in whom surgery was beneficial, namely: those with 3 diseased vessels and normal left ventricular function, those with proximal obstruction in the left anterior descending artery, those with ST-segment depression by more than 1.5 mm during exercise testing or with abnormal resting electrocardiogram, elderly patients or those with peripheral vascular disease. A metaanalysis of 7 randomized studies showed the consistency of these findings. It gathered information from 2649 patients and a significant reduction was observed in mortality after 5, 7, and 10 years in patients randomized to bypass surgery (surgical mortality: 10.2%, 15.8%, and 26.4%, respectively; medical treatment mortality: 15.8%, 21.7%, and 30.4%, respectively), with a relative risk (RR) of 0.61, 0.68, and 0.83. The benefit was proportional to the number of diseased vessels (3 vessels), the presence of left main coronary artery disease or left anterior descending coronary artery disease, deterioration of ejection fraction and symptoms or signs (on the exercise test) of myocardial ischemia.70 These studies have received much criticism because of the high degree of group interaction, the limited recruitment of women, the low use of arterial grafts, the low use of antiplatelet agents, and because they were done before aggressive management of cardiovascular risk factors. Even so, the findings are still considered valid because of their consistency and are of great use when indicating revascularization for prognostic purposes.
Revascularization in the Therapeutic Strategy for Stable Ischemic Heart Disease
Revascularization plays an important role in the therapeutic approach to stable angina. Thus, all patients with stable ischemic heart disease and 1) advanced functional class or symptoms that prevent them from leading a fulfilling life, 2) clinical findings suggestive of extensive coronary artery disease or deterioration in ventricular function (diabetes, prior infarction, history of heart failure), or 3) angina or coronary ischemia with complementary tests showing decreased ejection fraction (sometimes even below 50%), should undergo tests for detection and quantification of ischemia or estimation of myocardial viability in akinetic areas as applicable. The findings of these tests will determine the indication for coronary angiography with the goal to evaluate the possibility and type of revascularization.
Revascularization in the Therapeutic Strategy of NSTE-ACS
The therapeutic strategy of NSTE-ACS is complex and so algorithms have been developed to assist and simplify decisions.23-25 Three studies (FRISC II,20 TACTICS-TIMI 18,21 and RITA 322), conducted in recent years, have significantly changed the therapeutic strategy in patients with NSTE-ACS.
The first study to be published was the Scandinavian study FRISC II,20 which included 2457 patients with high risk NSTE-ACS. These patients were randomized to a classic conservative strategy or an invasive one in which cardiac catheterization and revascularization were performed between the second and seventh days. Of those patients assigned to invasive strategies, 34% underwent bypass surgery (the left mammary artery was used in 95% of the patients and mortality was only 2.1%) and 44% underwent percutaneous revascularization (66% with stenting and 10% received abciximab). The results were very favorable for those assigned to the interventional strategy. After 1 year,71 the incidence of death or reinfarction was 26% lower for those in the invasive treatment group (10.5% vs 14.2%; RR=0.76; 95% confidence interval [CI], 0.59-0.92) and mortality decreased by 44% (2.2% vs 4%; RR=0.6; 95% CI, 0.35-0.80). Moreover, the patients assigned to the invasive group showed a better clinical course after 6 months, with less need for medication to treat angina, better functional class and lower proportion of rehospitalization and lower probability of presenting angina.20 This study was therefore the one that clearly showed that patients with high-risk NSTE-ACS benefit more from an interventional strategy than from a conservative strategy. The second study, TACTICS-TIMI 18,21 confirmed the results of FRISC II. The study included 2220 patients with high-risk NSTE-ACS treated with tirofiban as well as with aspirin and sodium heparin. Catheterization in patients in the invasive treatment group was performed between 4 hours and 48 hours after hospital admission. After 6 months, the incidence of the composite event of death, reinfarction or rehospitalization for ACS (the primary study endpoint) was 22% lower in the group who underwent the intervention (15.9% vs 19.4%; odds ratio [OR]=0.78; 95% CI, 0.62-0.97). The last of the 3 studies that have changed the therapeutic approach to NSTE-ACS is the RITA 3 study,22 which enrolled 1810 patients with unstable angina and evidence of coronary heart disease. Patients were excluded if they had developed either a Q-wave myocardial infarction or creatine kinase MB levels twice the upper normal value. The incidence of death, myocardial infarction or refractory angina after 4 months (one of the 2 primary endpoints of the study) was significantly lower in the invention group (9.6% vs 14.5%; RR=0.66; 95% CI, 0.32-0.85). This difference was maintained after 12 months. Taken together, these 3 studies show that in patients with high-risk NSTE-ACS an invasive strategy with the current techniques is preferable to a conservative approach in terms of clinical outcome.
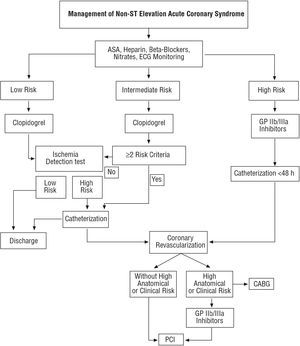
Revascularization therefore plays a key role in the management of NSTE-ACS. Analysis of the subgroups of the FRISC II20 and TACTICS21 studies has shown that the benefit is not the same for all patients. Some subgroups (patients at low risk) do not show any difference between conservative treatment and interventional treatment, highlighting the importance of an appropriate stratification to in order to apply interventional management in patients in whom real clinical benefit will be obtained (high or moderate risk). Thus, all patients with NSTE-ACS should be stratified23-25 and those at high risk (TIMI score ≥4,23 high risk according to the Spanish Society of Cardiology or moderate with 2 or more factors24 [Table 3], or high risk according to the European Society of Cardiology25) should undergo early coronary angiography and revascularization if the findings of the angiogram so indicate. The algorithm proposed by the Spanish Society of Cardiology is shown in Figure 4.
Figure 4. Algorithm proposed by the Spanish Society of Cardiology for management of non-ST elevation acute coronary syndrome according to risk stratification.24 ASA indicates acetylsalicylic acid; CABG, coronary artery bypass graft; GP, glycoprotein; PCI, percutaneous coronary intervention.
One aspect still to be resolved is the timing of the invasive evaluation in patients with NSTE-ACS for whom an invasive strategy is appropriate. In this regard, catheterization was done within 7 days in the FRISC20 study (median, 4 days), whereas in the TACICS-TIMI 1821 study, it was done between 4 hours and 48 hours (median 22 hours) and within 72 hours in the RITA 3 study,22 with a median of 2 days. Timing was analyzed specifically in 2 recent studies--the ELISA72 and the ISAR-COOL73--with contradictory results. The ELISA study randomized 220 patients with NSTE-ACS to early catheterization (<12 h) or late catheterization (24-48 h). Contradictory to the study hypothesis, the enzymatic infarct size was greater in the group assigned to early coronary angiography and intervention. This surprising observation was attributed to the patients who were assigned to early catheterization not receiving glycoprotein IIb/IIIa inhibitors. In the ISAR-COOL study,73 all patients were treated with tirofiban and the median time was 2.4 hours for the early group and 86 hours for the late group. The incidence of death or infarction after 30 days (primary study endpoint) was 11.6% in patients assigned to the group with delayed catheterization and 5.9% in the group assigned to early treatment. This difference occurred at the expense of events that occurred before catheterization. Therefore, it seems reasonable to carry out catheterization as soon as possible in patients at high risk, though this should not affect the initiation of optimal antithrombotic treatment.
Indications for Revascularization
The scientific societies have drawn up indications, both for coronary bypass surgery and PCI, based on the reviewed evidence of efficacy and effectiveness of revascularization, both for stable angina and for NSTE-ACS.39,40,74,75 The most up-to-date indications at present are those developed jointly by the American College of Cardiology and the American Heart Association (ACC/AHA) for surgery or PCI. These are summarized in Tables 5 to 9.
BYPASS SURGERY VERSUS PERCUTANEOUS CORONARY INTERVENTION: CLINICAL CONSIDERATIONS WHEN MAKING DECISIONS
As many as 9 randomized trials have been published, all in the second half of the nineties, comparing angioplasty and bypass surgery in patients with multivessel disease and proximal disease of the left anterior descending artery disease. Analysis of these trials showed no significant differences in mortality or the composite endpoint of death or myocardial infarction in the long term.76,77 However, there weferences in the need for new revascularization procedures in the first year (33.7% vs 3.3%) and patients who underwent bypass surgery had a lower incidence of angina in the first year of follow up. The biggest and most important study with the longest follow up and best design in this period was the BARI study,45 in which 1829 patients were randomized to PTCA or bypass surgery. After 5.4 years, no differences were found in the primary endpoint (overall mortality) although the incidence of need for further revascularization was 5 times greater in the PTCA group (54% vs 8%). In 2000, an extension to the BARI study was published78 with 7.8 years of follow up and a slight advantage in favor of bypass surgery for survival (94.4% vs 80.9%; P=.043) due to diabetic patients (survival of 76.4% vs 55.7%; P=.0011). All these studies have important limitations, such as they had to exclude a large proportion of patients (left main coronary artery disease, diffuse lesions, complete occlusion, ventricular dysfunction or inability to achieve complete revascularization) but, above all, the revascularization procedures, whether percutaneous or bypass, bare little resemblance to those currently performed (stents and new antiplatelet agents were not used and arterial conducts were little used in surgery). So although these studies represent an important step forward, revascularization in patients with multivessel disease should currently be evaluated from a modern perspective with an eye on its immediate future.
The first thing to have clear is that the choice of PCI or bypass surgery does not apply to all patients with multivessel coronary disease, but rather to a subgroup in whom it is possible to do a functionally acceptable revascularization, whether by bypass surgery or by angioplasty. There is a broad group of patients in whom percutaneous revascularization is not possible despite the obvious advances in PCI. The current outcome data of the 2 techniques in patients with multivessel disease come from 6 clinical trials published over the last 6 years that compare current bypass surgery with PCI that more closely resembles current technique (stenting and new antiplatelet agents) (Table 10). The ARTS study79--without doubt the most important--included 1205 patients and showed no differences in the composite incidence of death, infarction and stroke between the 2 approaches and after 1 year, although patients in the stent group had a greater need for an additional revascularization procedure (16.8% vs 3.5%), a difference that was even more marked among diabetic patients (22.3% vs 3.5%). Analysis of cost per patient favored stenting, with a net saving of $2973 per patient. In the last congress of the AHA in November 2004, the results after 5 years of follow up were presented.80 The incidence of death was similar between patients assigned to PCI and bypass surgery (8% vs 7.6%; P=.83; RR=1.05; 95% CI, 0.71-1.55), although a nonsignificant but clinically relevant trend was seen in the subgroup of diabetic patients towards higher mortality among patients treated with PCI (13.4% vs 8.3%; P=.27; RR=1.61; 95% CI, 0.71-3.63). In line with the results for 1 year, no differences were seen in mortality, rate of infarction or stroke (18% vs 15%; P=.14; RR=1.22; 95% CI, 0.95-1.58). The need for further revascularization procedures did, however, show group differences, being done 3 times more often in the group assigned to percutaneous revascularization (30% vs 9%; P<.001; RR=3.46; 95% CI, 2.61-4.60).
The second most important study was the Stent or Surgery (SoS) Trial,81 which enrolled 988 patients and followed them for a mean of 2 years. The number of revascularizations required was similar to the previous study (21% in the stent group vs 6% in the bypass surgery group). Mortality was higher in the group assigned to PCI, but this finding was confounded by an abnormally low mortality in the bypass surgery group and very high noncardiovascular mortality in the group assigned to stenting. The findings of the other current studies that compare surgery with PCI were consistent with these results, but the number of patients in these studies was smaller. The AWESOME study82 included 454 patients with a particularly high risk profile. Survival at 3 years was similar--79% in the bypass surgery group and 80% in the stent group.
The 2 approaches have also been compared in patients with isolated proximal disease of the left anterior artery in the SIMA study,83 with a population size of 121 patients randomized to bypass surgery with the internal mammary artery or revascularization with stenting. After 2.4 years, there were no differences in mortality, functional class, drug use or changes in quality of life, although the rate of new revascularizations was different, being more common in the stent group (31% vs 7%).
In summary, technical advances and greater experience have helped reduce but not eliminate the main difference between the 2 techniques, namely, the need for further revascularization procedures. The available follow up information suggests no advantage with respect to mortality, infarction or stroke, except in diabetic patients who continue to show greater long-term mortality with PCI. Therefore, the decision on the type of revascularization in patients with multivessel coronary artery disease should be taken on individual merits and with the participation of the patient. Obviously, concurrent diseases, which imply a higher surgical risk, favor percutaneous revascularization, as well as interventions in patients with ACS where fast revascularization of the infarct-related artery is a priority. In contrast, bypass surgery seems the first choice approach in patients little suited to the new PCI and who have a low surgical risk and, above all, in stable diabetic patients.
The immediate future may change this line of thinking substantially. The development and widespread use of drug-eluting stents that inhibit intimal hyperplasia have helped reduce the rates of restenosis, the main cause of repeat revascularization. Future clinical trials will answer whether this will lead to equilibrium between the two revascularization techniques. Initial findings are promising. Preliminary results from the ARTS II study were presented in the Transcatheter Cardiovascular Therapeutics (TCT) 2004 meeting (by Dr de Bruyne on September 30, 2004). This study compared 607 patients of similar characteristics to those included in the ARTS study with patients in the 2 groups of this preceding study (coronary bypass surgery or PCI with conventional stents). The patients who underwent PCI received sirolimus-eluting stents. After 6 months, not only mortality but also incidence of myocardial infarction or stroke were similar in the 3 groups, and the rate of further revascularization procedures for multivessel angioplasty with sirolimus-eluting stents was similar to that of bypass surgery and less than that of PCI with conventional stents. Event-free survival from major cardiac events was 94% in patients undergoing PCI with drug-eluting stents and 91% in those who underwent bypass surgery, whereas those assigned to PCI with conventional stents had an event-free survival of 80%.
Section Sponsored by Laboratorio Dr Esteve
Correspondence: Dr. J.J. Alonso.
Hospital de Fuenlabrada. Servicio de Cardiología.
Camino del Molino, 2. 28942 Fuenlabrada (Madrid). España.
E-mail: jalonso.hflr@salud.madrid.org