A 68-year-old man with a history of type 2 diabetes, dyslipidemia and hyperuricemia had been recently started on allopurinol. He was admitted to our hospital with a diagnosis of severe allopurinol-induced Stevens-Johnson syndrome and started on systemic corticotherapy with a favorable clinical response.
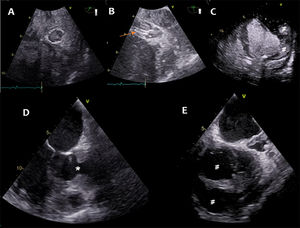
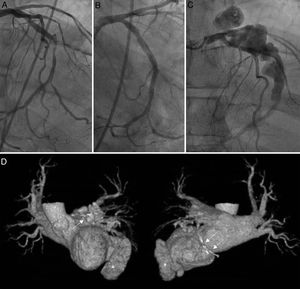
On day 10, the patient developed chest pain and hypotension and an electrocardiogram showed atrial fibrillation with complete heart block and inferoposterolateral ST-segment elevation. Emergent coronary angiography using the right femoral artery showed a critical stenosis in the middle segment of a dominant left circumflex artery (LCx). Percutaneous coronary intervention (PCI) with direct implantation of an everolimus-eluting stent (Xience Alpine 3.0 x 23mm, Abbott, United States) was performed with good angiographic result. On day 11, the patient developed fever and laboratory tests showed a marked increase in C-reactive protein (400 mg/L). Empirical broad spectrum antibiotic therapy was started. The patient was in Killip class II with a peak high-sensitivity troponin I (hs-TpI) of 14.483 ng/L. Transthoracic echocardiogram showed mild left ventricle (LV) dysfunction with inferoposterior akinesis, grade 2 functional mitral regurgitation, and small-volume pericardial effusion with no signs of vegetations. Persistent psychomotor agitation was interpreted in the context of acute disease because cerebral computed tomography (CT) was unremarkable. In the following days, the patient showed persistent fever and periods of respiratory distress requiring noninvasive ventilation. Serial hs-TpI showed a re-elevation from 2.100 to 14.483 ng/L. On day 15, antibiotic therapy was de-escalated to flucloxacillin after 2 positive cultures for methicillin-sensitive Staphylococcus aureus. Despite adequate antibiotic therapy, the patient maintained a fever and methicillin-sensitive S. aureus bacteremia. Contrast transesophageal echocardiography showed a heterogenous cavity compatible with a LCx aneurysm and a complex LV pseudoaneurysm in the posterolateral wall (figure 1). Coronary angiography showed a massive LCx aneurysm in the proximal and middle segments not limited to the area covered by the stent (figure 2 and video 1 of the supplementary data [coronary angiography showing the left circumflex artery aneurysm in multiple projections]). Cardiac CT further detailed the anatomy of the complex LV pseudoaneurysm with anterolateral and inferolateral cavities (figure 2 and video 2 of the supplementary data [cardiac computed tomography 3D reconstruction of the heart showing the left circumflex artery aneurysm and LV pseudoaneurysm]). A diagnosis was established of LCx mycotic coronary aneurysm (MCA) and LV pseudoaneurysm due to contained myocardial rupture. The clinical case was discussed in a Heart Team session and deemed unsuitable for surgical repair. In the following days, the patient showed progressive obnubilation and he eventually died. Informed consent for the purpose of publishing this case report was obtained from the patients’ family.
Contrast transesophageal echocardiography showing blood flow in an enlarged left circumflex artery with heterogenous walls (A,B), the implanted stent (arrow) and the LV pseudoaneurysm with a horseshoe distribution around the ventricle (#) arising from the posterolateral wall (*) (C-E).
Sequence of coronary angiography images showing left circumflex artery (LCx) stenosis (A), immediate postpercutaneous coronary intervention angiographic result (B), and subsequent LCx aneurysm (C). Panel D shows selected views of a 3-dimensional 360° cardiac CT reconstruction of the heart where the LCx aneurysm (arrows) and the left ventricle pseudoaneurysm (*) are visualized. Left anterior oblique 0° angiographic projections.
MCAs are a very rare complication of PCI. Few cases of MCA with associated complications have been reported in the literature, particularly those in which multimodality imaging allowed full anatomical characterization.1 Mechanical factors associated with arterial wall injury caused by stent deployment, local immunosuppression and systemic corticotherapy have been described as contributing factors.2 MCA are formed by microbial invasion and destruction of the vessel wall. The most common agent is S. aureus. MCAs have a poor prognosis, with a recent case series describing a 43% fatality rate and complications such as myocardial infarction, purulent pericardial effusion, and ventricular rupture.2,3 Diagnosis is challenging, requiring a high degree of suspicion and multimodality imaging. Treatment is individualized and depends on the clinical presentation, MCA extension, and associated complications. The most common treatment option is antibiotic therapy and surgical excision with distal bypass.3
In this clinical case, we hypothesize that the stent provided a nidus for methicillin-sensitive S. aureus in the context of persistent bacteremia and systemic corticotherapy. The patient likely developed bacteremia secondary to the multiple skin lesions caused by Stevens-Johnson syndrome. Multimodality imaging with transesophageal echocardiography, cardiac CT and coronary angiography were required for full anatomical definition and decision-making. Treatment options were limited in the context of complex coronary and ventricular lesions which would have required MCA excision with distal bypass and ventriculoplasty.
FUNDINGNone declared.
AUTHORS’ CONTRIBUTIONSP. G. Diogo drafted the first manuscript. C. X. Resende provided detailed revision of the manuscript. S. Torres interpreted and provided the transesophageal echocardiography images. M. Vasconcelos interpreted the cardiac CT images and provided the 360° reconstructions. R. Pinto provided the coronary angiography videos. All authors were actively involved in this clinical case, have reviewed the manuscript, and approved its submission.
CONFLICTS OF INTERESTNone declared.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.09.009