We present the case of a 68-year-old woman, who was under follow-up for chronic right heart failure, with aortic and mitral prostheses implanted at age 34 and 51 years, respectively. She had a 7-year history of progressive tricuspid valve dysfunction, with severe regurgitation, moderate pulmonary hypertension, and symptoms of being easily fatigued, gastric fullness, and edema that was difficult to control with medical treatment. The multidisciplinary team considered the surgery to be high risk and opted for repair with a MitraClip device.
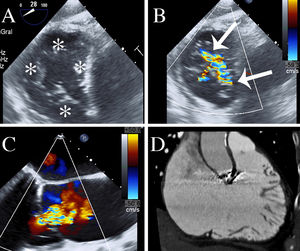
The procedure was planned using transthoracic and transesophageal echocardiography, which identified a nonthickened tricuspid valve, composed of 4 leaflets, 2 of which were posterior, 1 septal, and 1 anterior (Figure 1A, asterisks). The regurgitation was secondary to dilatation of the ring, and extended along the entire line of valvular coaptation (Figure 1B and C, arrows). The workup was completed with cardiac computed tomography (Figure 1D) and magnetic resonance imaging. These showed severe tricuspid regurgitation with a regurgitant fraction of 48% (45mL), moderate right ventricular dilatation (113mL/m2), and an ejection fraction at the lower limit of normality (56%).
Multimodality imaging in the planning stage. A and B: TEE in transgastric plane on which the 4 valve scallops (asterisks) and a large jet are seen. C: TEE in midesophageal plane at 160°, showing the severity of the regurgitation. D: right ventricular plane on CT showing ventricular dilatation. CT, computed tomography; TEE, transesophageal echocardiography.
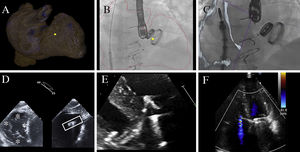
The procedure was performed under multimodal imaging guidance (video,supplementary material). HeartNavigator was used for fusion of computed tomography with fluoroscopy (Figure 2A and B), despite the limitation of this technique for mobile structures such as valve leaflets. Nonetheless, it allows the limits of the structures adjacent to the tricuspid valve to be ascertained. Right ventricular and atrial dilatation are associated with distortion of the normal anatomy. Establishing the spatial position of the caval axis, the right atrial appendage (area of interference with guide), the tricuspid ring and the ventricular apex orientates the interventional cardiologist during the procedure. A marker identified the desired clip position between the septal and anterior leaflets.
Multimodal imaging during implantation. Fusion of images with computed tomography (A-B); the marker that identified the desired clip position can be seen between the septal and anterior leaflets (yellow dot). C: fusion of images with echocardiography. D: echocardiography to assess coaxiality. E: grasping. F: final result.
Three-dimensional reconstruction (Figure 2A) helped identify the different structures on fluoroscopy. The outer border of the segmented structures was projected onto the screen (Figure 2B) with the aim of allowing the catheters to be moved safely in the atrium. The EchoNavigator was also used for fusion of the transesophageal images with fluoroscopy. The visualization of the caval axis in real time (Figure 2C) allowed the catheter to be moved to aim it toward the tricuspid valve.
Once the clip was centered on the valve, we checked its coaxiality with the line of coaptation between the septal and anterior scallops. Simultaneous biplanar acquisition was used with vertical inclination, rather than the usual horizonal inclination that shows 2 orthogonal planes, from a transgastric position (Figure 2D). The 40° plane showed the valve scallops (Figure 2D left, asterisks) and the simultaneous plane was parallel, with 23° vertical inclination. This second plane showed the orientation of the clip (Figure 2D right, box). Good coaxiality of the device to the septal-anterior scallops was identified (Figure 2D, orientation of the box), albeit in a posterior position, which was corrected.
Leaflet grasping could not been seen adequately on the transesophageal window. Therefore, we opted to change to transthoracic echocardiography, which revealed that the septal leaflet had not been grasped and there was tricuspid regurgitation between the clip and the leaflet. Grasping was therefore done with transthoracic echocardiographic guidance, and was successful on the third attempt, with good visualization of the grasp (Figure 2E). Next we checked the indirect signs of adequate leaflet grasping, as in a mitral clip procedure, which were favorable. The regurgitation was reduced from severe to mild (Figure 2F) and the patient progressed well. One month later, magnetic resonance imaging showed reduction of right ventricular volume to 77mL/m2, reduction of the regurgitant fraction to 19% and a preserved ejection fraction of 60%. Follow-up at 4 months showed significant clinical improvement with reduction of diuretic use.
Severe tricuspid regurgitation is a condition that is often related to surgically-corrected left-sided valve disease, and has a poor long-term prognosis.1 Transcatheter treatment can nowadays be studied with a multitude of devices that act at different levels.2 Multimodal imaging plays an important role in the continuity of the process. It is key to understanding the functional anatomy of the lesion and personalize the repair, which means optimal patient selection. The vast experience with MitraClip has made it the first tested device, independently of the regurgitation mechanism, with a 13% residual severe regurgitation rate.3 The Spanish experience so far is based on 2 cases4; here we present the first to show the usefulness of using the maximum commercially-available technology for patient selection, planning, and follow-up.
In conclusion, multimodal imaging provides precision and safety in the process of patient selection, implant guidance, and subsequent follow-up.
CONFLICTS OF INTERESTC.-H. Li and D. Arzamendi have received honoraria from Abbott.