Superior sinus venosus defect (SVD) is a rare congenital heart disease accounting for 5% to 10% of all cases of atrial septal defect.Transcatheter correction of SVD using covered Cheatham-Platinum stents (NuMED, United States) has emerged as an alternative to open-heart surgery.1–3 The 50- and 60-mm long stents subsequently received Conformite Europeenne marking and Food and Drug Administration approval. However, the anatomical configuration of SVD often requires a stent longer than 60mm, which are currently unavailable in many countries.3 The Optimus XXL stent (AndraTec GmbH, Germany) is a nonpremounted, balloon-expandable, cobalt-chrome, extra large stent, used for endovascular stenting of aortic coarctation or for right ventricle outflow tract stenting.4 A covered 99-mm long version was specifically developed for SVD correction, as recently reported in one case.5
We report a multicenter case serie of 6 additional consecutive cases achieved in 3 centers in 2 countries between November 2021 and March 2022 in adults aged 26 to 72 years. The study design was approved by an ethics committee (GERM, IRB00012157). Informed consent was obtained from the patients.
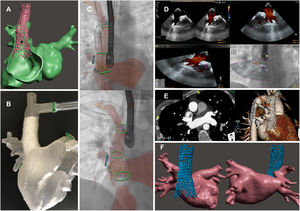
Patient and procedural characteristics are reported in table 1. All patients complained of dyspnea and had significant left-to-right shunt. High opening of the anomalous pulmonary venous return in the superior vena cava (SVC) was idenfied in 4 cases. Procedural feasibility was tested on virtual simulation in all patients and hands-on simulation training in 4 (figure 1).6 To define the best treatment option, a multidisciplinary team including heart surgeons assessed the imaging and simulation processes. Transcatheter correction was considered as an alternative to surgery in all patients. As previously described,1–3,6 all procedures were performed under general anesthesia and transesophageal echocardiography guidance. Multimodal fusion imaging was applied in 5 patients (figure 1). A venous femoro-jugular rail was used. Transseptal access was employed to establish an anomalous pulmonary venous return pathway in 5 patients, with balloon inflation simultaneous to Optimus stent deployment in 4.
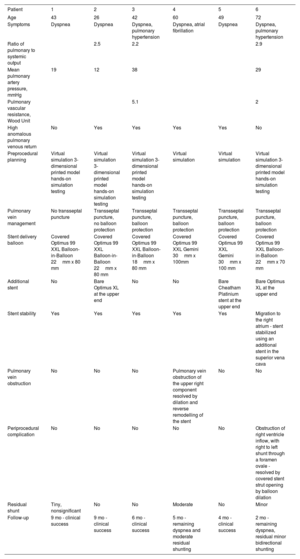
Description of patients’ characteristics, procedural data and outcomes.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Age | 43 | 26 | 42 | 60 | 49 | 72 |
| Symptoms | Dyspnea | Dyspnea | Dyspnea, pulmonary hypertension | Dyspnea, atrial fibrillation | Dyspnea | Dyspnea, pulmonary hypertension |
| Ratio of pulmonary to systemic output | 2.5 | 2.2 | 2.9 | |||
| Mean pulmonary artery pressure, mmHg | 19 | 12 | 38 | 29 | ||
| Pulmonary vascular resistance, Wood Unit | 5.1 | 2 | ||||
| High anomalous pulmonary venous return | No | Yes | Yes | Yes | Yes | No |
| Preprocedural planning | Virtual simulation 3-dimensional printed model hands-on simulation testing | Virtual simulation 3-dimensional printed model hands-on simulation testing | Virtual simulation 3-dimensional printed model hands-on simulation testing | Virtual simulation | Virtual simulation | Virtual simulation 3-dimensional printed model hands-on simulation testing |
| Pulmonary vein management | No transseptal puncture | Transseptal puncture, no balloon protection | Transseptal puncture, balloon protection | Transseptal puncture, balloon protection | Transseptal puncture, balloon protection | Transseptal puncture, balloon protection |
| Stent delivery balloon | Covered Optimus 99 XXL Balloon-in-Balloon 22mm x 80 mm | Covered Optimus 99 XXL Balloon-in-Balloon 22mm x 80 mm | Covered Optimus 99 XXL Balloon-in-Balloon 18mm x 80 mm | Covered Optimus 99 XXL Gemini 30mm x 100mm | Covered Optimus 99 XXL Gemini 30mm x 100 mm | Covered Optimus 99 XXL Balloon-in-Balloon 22mm x 70 mm |
| Additional stent | No | Bare Optimus XL at the upper end | No | No | Bare Cheatham Platinium stent at the upper end | Bare Optimus XL at the upper end |
| Stent stability | Yes | Yes | Yes | Yes | Yes | Migration to the right atrium - stent stabilized using an additional stent in the superior vena cava |
| Pulmonary vein obstruction | No | No | No | Pulmonary vein obstruction of the upper right component resolved by dilation and reverse remodelling of the stent | No | No |
| Periprocedural complication | No | No | No | No | No | Obstruction of right ventricle inflow, with right to left shunt through a foramen ovale - resolved by covered stent strut opening by balloon dilation |
| Residual shunt | Tiny, nonsignificant | No | No | Moderate | No | Minor |
| Follow-up | 9 mo - clinical success | 9 mo - clinical success | 6 mo - clinical success | 5 mo - remaining dyspnea and moderate residual shunting | 4 mo - clinical success | 2 mo - remaining dyspnea, residual minor bidirectional shunting |
Clinical case 1. A 43-year-old man with SVD. A: computer simulation of Optimus stent implantation. B: hands-on simulation testing. C: stent implantation under fusion imaging guidance. D: color Doppler flow showing a widely patent pulmonary vein channel toward the left atrium. E and F: cardiac tomography confirms excellent position of the stent, complete occlusion of the SVD and widely patent pulmonary vein channel.
In 2 patients, a single size (outer/inner balloon of 30/14-mm diameter and 100-mm length) Gemini balloon-in-balloon was used to implant the stent (AndraTec GmbH, Germany). The maximum diameter of this ballon was larger than the SVC diameter. In 4 patients, the single size 100-mm length Gemini balloon was not chosen given a too large diameter and other 20 to 30mm shorter balloon-in-balloon stents were used (NuMED, United States), with an outer balloon diameter between 18 to 22mm to match the diameter of the SVC (figure 1). This setting required additional inflations of the extremities of the stent that were not fully expanded by the smaller balloons. A second uncovered stent was implanted at the upper part of the stent in 3 patients to provide additional anchoring to the SVC.
In 4 patients, we achieved technical and clinical success. One procedure was marked by pulmonary vein obstruction reversed by pulmonary vein balloon dilation but leading to residual shunting and persistant dyspnea. One of the 4 patients in whom a shorter balloon-in-balloon was used was complicated by displacement of the stent toward the right atrium. The stent was subsequently anchored in the SVC using another uncovered stent and struts of the Optimus stent had to be opened to restore flow toward the right ventricle. In this patient, a modified suture control technique may have been useful to secure the stent position before full stent deployment and impaction on SVC was obtained.5 Outcome was favorable. Unadequate diameter or length of the balloon-in-balloon contributed to these 2 complications.
Transcatheter correction of a SVD using a covered Optimus XXL 99-mm stent was feasible in all 6 patients. The strengths of the Optimus stent are its adequate length and high comformability. This allows deep and stable implantation in the SVC, whereas its good flexibility allows optimal flaring of the the proximal part of the end of the stent to achieve complete shunt closure. When the area of stent implantation in the SVC is too short, the stent may migrate, as observed in 1 patient. A modification of the Optimus stent with a longer uncovered part at the upper end was performed to address this issue and strengthen the anchoring in the SVC. Currently available Gemini balloons with multiple balloon sizes will also optimize stent implantation.
To conclude, the Optimus covered, 99 mm-long, Optimus XXL stent allows successful transcatheter SVD. Further experience and a wider range of stent/balloons are needed.
FUNDINGMarie Lannelongue Department of Research and Innovation, 3D Heart Modeling Co (Caissargues, France), the nonprofit organisation Le coeur dans la main, a grant of the Federation Francaise de Cardiologie and a Bourse Hélène de Marsan grant from the French Society of Cardiology
AUTHORS’ CONTRIBUTIONSC. Batteux, and V. Ciobotaru participated in the study design and preclinical testing. C. Batteux, V. Ciobotaru, H. Bouvaist, A. Kempny, A. Fraisse and S. Hascoet participated in the clinical cases and data collection. S. Hascoet and A. Fraisse drafted the manuscript. All authors critically revised the manuscript.
CONFLICTS OF INTERESTS. Hascoet has received proctoring and consultant fees from Abbott and a research grant from Edwards lifesciences. A. Fraisse has received proctoring and consultant fees from Abbott and Occlutech. A. Kempny, H. Bouvaist, C. Batteux and V. Ciobotaru have no disclosures.
We thank A. Wolfe, M. Gatzoulis, P. Brenot, W. Arditi, J. Radojevic, B. Decante, W. Li, F. Lecerf, C. Lacerda, G. Albenque, L. Aubrege, H. Beaussier and F. Rémy for their contribution to this work.