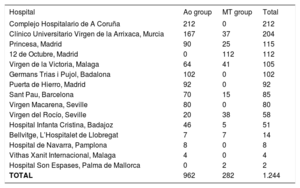
Minimally invasive surgery is performed in many Spanish centers, but few articles give the impression that these techniques are widely used in Spain.1,2 We present an analysis of the data compiled in a Spanish registry including 15 centers where minimally invasive surgery is performed, mainly for aortic valve replacement and mitral valve repair or replacement (Table 1).
Centers Participating in the Registry, With the Number of Patients Included per Center
| Hospital | Ao group | MT group | Total |
|---|---|---|---|
| Complejo Hospitalario de A Coruña | 212 | 0 | 212 |
| Clínico Universitario Virgen de la Arrixaca, Murcia | 167 | 37 | 204 |
| Princesa, Madrid | 90 | 25 | 115 |
| 12 de Octubre, Madrid | 0 | 112 | 112 |
| Virgen de la Victoria, Malaga | 64 | 41 | 105 |
| Germans Trias i Pujol, Badalona | 102 | 0 | 102 |
| Puerta de Hierro, Madrid | 92 | 0 | 92 |
| Sant Pau, Barcelona | 70 | 15 | 85 |
| Virgen Macarena, Seville | 80 | 0 | 80 |
| Virgen del Rocío, Seville | 20 | 38 | 58 |
| Hospital Infanta Cristina, Badajoz | 46 | 5 | 51 |
| Bellvitge, L’Hospitalet de Llobregat | 7 | 7 | 14 |
| Hospital de Navarra, Pamplona | 8 | 0 | 8 |
| Vithas Xanit Internacional, Malaga | 4 | 0 | 4 |
| Hospital Son Espases, Palma de Mallorca | 0 | 2 | 2 |
| TOTAL | 962 | 282 | 1.244 |
Ao group, valve replacement alone, using a miniaccess; MT group, right anterior minithoracotomy for mitral replacement/repair, tricuspid repair, atrial septal defect closure, or atrial myxoma resection
In total, 1245 patients undergoing on-pump surgery were analyzed. Aortic valve replacement was performed using a ministernotomy as the preferred approach in 963 patients (Ao group) and mitral valve replacement, mitral repair, or another procedure was performed using a right anterior minithoracotomy in 282 patients (MT group).
The preoperative variables in both groups are shown in Table 2. The preferred technique in the Ao group was a ministernotomy, used in 945 patients (98%), which consisted of a vertical incision measuring 6 to 12cm (in 75%, 7–8cm) in the most cephalad portion of the sternum. Only 2% underwent surgery using a right anterior minithoracotomy approach, described as being as effective as ministernotomy for aortic valve replacement, but technically more demanding.3
Preoperative Characteristics and Results Obtained in Patients Treated Using Miniaccess Techniques
| Ao group | MT group | |
|---|---|---|
| Patients, n | 963 | 282 |
| Age, y | 75 [67-80] | 60 [49-69] |
| HT | 75 | 29 |
| Diabetes mellitus | 27 | 9 |
| Dyslipidemia | 62 | 19 |
| COPD | 15 | 7 |
| Peripheral arterial disease | 8 | 0.4 |
| Renal failure | 8 | 3 |
| Previous stroke | 5 | 4 |
| Normal ejection fraction | 87 | 89 |
| Moderately reduced ejection fraction | 12 | 8.2 |
| Severely reduced ejection fraction | 1.5 | 1.1 |
| Logistic EuroSCORE | 5 [3-7] | 2.7 [1.5-6.8] |
| EuroSCORE II | 2 [1-3] | 1.7 [0.8-2.3] |
| Size of incision, cm | 8 [7-9] | 7 [6-8.5] |
| Duration extracorporeal circulation, min | 81 ± 31 | 123 ± 45 |
| Duration aortic clamping, min | 61 ± 23 | 81 ± 42 |
| ICU stay, days | 3 ± 5 | 3 ± 6 |
| Total hospital stay, d | 10 ± 10 | 10 ± 8 |
| Reoperation for bleeding | 2.80 | 3.90 |
| Number packed red blood cell units transfused | 1 ± 1.8 | 0.7 ± 1.4 |
| Postoperative low cardiac output | 4 | 3.9 |
| Perioperative AMI | 0.2 | 1.4 |
| Pulmonary complications | 6 | 5 |
| Postoperative atrial fibrillation | 24 | 9.6 |
| Pacemaker requirement | 4.7 | 2.5 |
| Neurological complications | 3.2 | 2.5 |
| Postoperative renal failure | 8.2 | 3.9 |
| Surgical wound infection | 1.8 | 1.8 |
| Absence of periprosthetic aortic regurgitation | 96 | |
| Mild periprosthetic aortic regurgitation | 3.7 | |
| Moderate periprosthetic aortic regurgitation | 0.6 | |
| Severe periprosthetic aortic regurgitation | 0 | |
| Moderate postrepair mitral regurgitation | 0.4 | |
| Severe postrepair mitral regurgitation | 0 | |
| Moderate periprosthetic mitral regurgitation | 0 | |
| Severe periprosthetic mitral regurgitation | 0 | |
| Total mortality | 1.5 | 2.2 |
AMI, acute myocardial infarction; Ao group, aortic valve replacement alone, using a miniaccess; COPD, chronic obstructive pulmonary disease; HT, hypertension; ICU, intensive care unit; MT group, right anterior minithoracotomy for mitral replacement/repair, tricuspid repair, atrial septal defect closure, or atrial myxoma resection
Values are expressed as the percentage, mean ± standard deviation, or median [interquartile range].
Patients in the MT group underwent surgical treatment through a right anterior minithoracotomy for the following purposes: mitral valve replacement in 48%, mitral valve repair in 27%, closure of an atrial septal defect in 15%, and myxoma resection in 5%. The tricuspid valve was treated in 10% of patients.
The procedure-related information and data on morbidity and mortality in both groups are shown in Table 2. The revision rates for bleeding were low (Ao, 2.80% and MT, 3.90%). The rate of surgical wound infections was also reduced, with a value of only 1.80% in both groups.
Current technological advances, such as transesophageal echocardiography (regularly used in many types of cardiac procedures in almost all centers performing cardiac surgery), new instrumentation specifically designed for small approaches, and thoracoscopy techniques that provide excellent vision, have allowed the development of miniaccess surgery without increasing operative risk. Aortic and mitral valve surgery using small incisions has several advantages: lower bleeding rates, transfusion requirements, and wound infection rates; fewer respiratory complications; and shorter intensive care unit stay and overall length of hospital stay.4 The pioneers of the technique in Cleveland analyzed 832 patient pairs5 and found no significant differences in mortality, which was very low (0.96% in both groups). However, they reported differences in the number of bleeding episodes, transfusions, respiratory complications, and the percentage of patients extubated in the operating room in the ministernotomy group, as well as postoperative pain reductions, shorter hospital stay, and shorter duration of on-pump circulation and aortic clamping. Furthermore, all these advantages imply a significantly lower in-hospital cost expenditure per patient.
Similar advantages have been described for the MT approach, which is associated with reductions in morbidity and mortality, length of hospital stay, and repeat interventions for bleeding, as well as less pain, faster recovery, and, of course, evident aesthetic advantages that are particularly appreciated by younger patients.6
In the database analyzed, mortality in the Ao group was lower than would be expected attending to the logistic EuroSCORE and EuroSCORE IIrisk scores: the median [interquartile range] was 1.5% vs 5 [3-7] and 2 [1-3], respectively. Similar results were found in the MT group, which had an observed mortality of 2.20%, whereas the expected mortality was 2.7% [1.5-6.8] for the logistic EuroSCORE and 1.7% [0.8-2.3] for EuroSCORE II.
An analysis of the patients undergoing surgery starting from 2014 showed an even greater reduction in mortality. In the Ao group, the observed mortality was 1.2% whereas the expected mortality was 5.86% [3.40-8.44] according to the logistic EuroSCORE and 1.76% [1.16-2.87] according to EuroSCORE II. There were similar findings in the MT group, where the observed mortality starting from 2014 was 1.6%%, whereas the median risk was 2.08% [0.98-4.38] determined by the logistic EuroSCORE and 1.76% [0.98-2.48] by EuroSCORE II.
To conclude, these results indicate that miniaccess surgery is safe in Spain. In the coming years, we may see a significant expansion of this practice, which would benefit many patients, allowing faster return to normal activities of daily life, and with a lower cost expenditure for the publically-funded health care system.
We are grateful to the members of the Working Group for Minimally Invasive Surgery of the Spanish Society of Thoracic-Cardiovascular Surgery for their invaluable help in developing this scientific letter.