Current clinical practice guidelines do not recommend the use of statins in heart failure (HF).1 This recommendation is supported by 2 trials that studied hydrophilic statins.2,3 We conducted a retrospective study of patients admitted with HF between December 2007 and June 2011 to Hospital de Santa Tecla, Spain. The primary objective was to analyze the usefulness of lipophilic statins in these patients and the secondary objective was to compare real use with the theoretical indication for statins. Exclusion criteria were patients younger than 18 years or older than 85 years, those with neoplastic, infectious, or end-stage disease, and those receiving hydrophilic statins. We reviewed 680 patients, and considered only the first admission in patients who were re-admitted during the study. We compared patients receiving lipophilic statins with those not receiving any statins, and we calculated the percentage of patients who fulfilled the theoretical indications for receiving statins in accordance with the European Society of Cardiology Guidelines for the management of dyslipidemias.4 Quantitative variables are expressed as mean ± standard deviation, and data were compared with the Student t test or ANOVA. We used the chi-square test to compare qualitative variables, the Mann-Whitney test for nonparametric data, and logistic regression for the multivariable analysis. The SPSS package version 20.0 was used for the statistical analysis. Statistical significance was defined as P<.05.
A total of 270 patients were enrolled (Table 1). Compared with the nonstatin group, the statin group had lower levels of low-density lipoprotein cholesterol (LDL-C) (80±25mg/dL vs 98±35mg/dL; P=.01), hemoglobin (11.6±1.9g/L vs 12.2±2.2g/L; P=.04), and glomerular filtration rate (55.2±23mL/min/m2 vs 61.5±26mL/min/m2; P=.04). There was a higher prevalence of treatment with aspirin, clopidogrel, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in the statin group than in the nonstatin group (45.4% vs 26.5%; P=.01; 33.6% vs 13.5%; P<.001; and 76.1% vs 53%; P=.01, respectively). The statin group also had a higher prevalence of hypertension, diabetes mellitus and dyslipidemia, and HF of ischemic etiology. There were no differences in cardiovascular or all-cause mortality or re-admission (Table 2). A multivariable regression was performed, adjusting for age, sex, hypertension, diabetes mellitus, dyslipidemia, HF of ischemic etiology, glomerular filtration rate (< 60mL/min/m2), anemia (hemoglobin<12 g/L) and LDL-C (< 80mg/dL). We found that lipophilic statins were not associated with cardiovascular mortality (odds ratio [OR]=1.12; 95% confidence interval [95%CI], 0.22-5.64; P=.88) or all-cause mortality (OR=4.94; 95%CI, 0.90-27.11; P=.06), or with cardiovascular re-admission (OR=0.91; 95%CI, 0.63-1.34; P=.66) or all-cause re-admission (OR=1.06; 95%CI, 0.82-1.38; P=.61). In theory, at least 84.9% of the study patients should have been receiving statin therapy, but in practice, this figure was 40.9%.
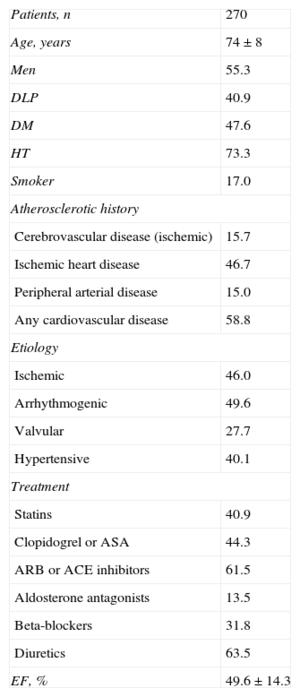
Characteristics of the Study Patients
| Patients, n | 270 |
| Age, years | 74±8 |
| Men | 55.3 |
| DLP | 40.9 |
| DM | 47.6 |
| HT | 73.3 |
| Smoker | 17.0 |
| Atherosclerotic history | |
| Cerebrovascular disease (ischemic) | 15.7 |
| Ischemic heart disease | 46.7 |
| Peripheral arterial disease | 15.0 |
| Any cardiovascular disease | 58.8 |
| Etiology | |
| Ischemic | 46.0 |
| Arrhythmogenic | 49.6 |
| Valvular | 27.7 |
| Hypertensive | 40.1 |
| Treatment | |
| Statins | 40.9 |
| Clopidogrel or ASA | 44.3 |
| ARB or ACE inhibitors | 61.5 |
| Aldosterone antagonists | 13.5 |
| Beta-blockers | 31.8 |
| Diuretics | 63.5 |
| EF, % | 49.6 ± 14.3 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; ASA, acetylsalicylic acid; DLP, dyslipidemia; DM, diabetes mellitus; EF, ejection fraction; HT, hypertension; NYHA, New York Heart Association functional class.
Data are expressed as a percentage or mean±standard deviation, unless otherwise indicated.
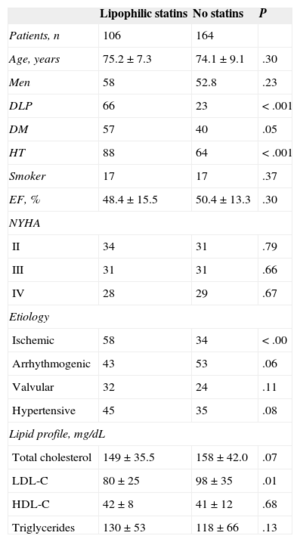
Clinical Data and Lipid Profile of Patients Receiving Lipophilic Statins and Those not Receiving Statins
| Lipophilic statins | No statins | P | |
|---|---|---|---|
| Patients, n | 106 | 164 | |
| Age, years | 75.2±7.3 | 74.1±9.1 | .30 |
| Men | 58 | 52.8 | .23 |
| DLP | 66 | 23 | <.001 |
| DM | 57 | 40 | .05 |
| HT | 88 | 64 | <.001 |
| Smoker | 17 | 17 | .37 |
| EF, % | 48.4±15.5 | 50.4±13.3 | .30 |
| NYHA | |||
| II | 34 | 31 | .79 |
| III | 31 | 31 | .66 |
| IV | 28 | 29 | .67 |
| Etiology | |||
| Ischemic | 58 | 34 | <.00 |
| Arrhythmogenic | 43 | 53 | .06 |
| Valvular | 32 | 24 | .11 |
| Hypertensive | 45 | 35 | .08 |
| Lipid profile, mg/dL | |||
| Total cholesterol | 149±35.5 | 158±42.0 | .07 |
| LDL-C | 80±25 | 98±35 | .01 |
| HDL-C | 42±8 | 41±12 | .68 |
| Triglycerides | 130±53 | 118±66 | .13 |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; DLP, dyslipidemia; DM, diabetes mellitus; EF, ejection fraction; HT, hypertension; NYHA, New York Heart Association functional class;.
Data are expressed as a percentage or mean±standard deviation, unless otherwise indicated.
This study has similar characteristics to those reported in recent studies in our setting.5 The higher prevalence of hypertension, diabetes mellitus, dyslipidemia, and HF of ischemic etiology in patients receiving lipophilic statins is probably explained by worse underlying atherosclerosis. In fact, 58.8% of all patients had already experienced an ischemic event before admission. Both the lower glomerular filtration rate and the higher prevalence of antiplatelet agents and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers can be similarly explained. Patients receiving lipophilic statins had lower LDL-C levels, but these levels did not result in improved clinical outcome. While statins do indeed prevent the onset of ischemic events, there is also a known association between very low cholesterol levels and lower survival in HF.1 Furthermore, anemia is associated with more re-admissions and lower survival in elderly, hospitalized patients with HF,1 an association corroborated by our study. The multivariable regression analysis showed no association between lipophilic statins and lower cardiovascular or all-cause re-admissions or mortality. The equivalent mean atorvastatin dose in our study (54.6 mg) may not have been high enough to produce evidence of these benefits, because a post hoc analysis of high-dose lipophilic statins found that they do appear to be useful in HF.6 Evidence of lower re-admission rates for HF reported with hydrophilic statins2 means that we should reconsider whether statin solubility plays a role in this context. Finally, only 40.9% of patients in our study were receiving statin therapy, which is much lower than the 85.9% calculated according to current guidelines for the management of dyslipidemias.4
In light of these results, it appears reasonable to maintain statin therapy at least in patients with HF of atherosclerotic origin.