Keywords
INTRODUCTION
Pacing with single-lead VDD pacemakers in complete atrioventricular block (CAVB) has been shown to be safe and effective in a number of studies. Atrial undersensing is a disadvantage, but appears to have no relevant clinical repercussions.1 Nevertheless, the physiopathological changes caused by atrial undersensing can lead to RR oscillations, which may trigger torsade de pointes (TdP) in the context of abnormal repolarization.
We describe 3 patients with a single-lead VDD pacemaker, normal cardiac function, no ion abnormalities, and no intake of QT-prolonging agents. An intermittent atrial sensing malfunction led to bradycardia, sudden RR oscillations, and the appearance of episodes of syncope due to TdP in all 3 patients. The retrospective analysis revealed noticeable QT interval prolongation in the electrocardiograms (ECG) with CAVB. The importance of this finding is discussed.
CASE DESCRIPTIONS
Patient 1
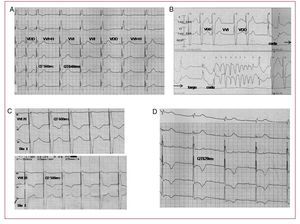
An 81-year-old woman had received a single-lead VDD pacemaker (Vitatron Saphir 3) for CAVB; sinus rhythm at 90 bpm was recorded prior to implantation. At 2 weeks, she consulted for 3 episodes of syncope. The ECG on admission showed pacemaker mode changes with switching to VVI after loss of atrial sensing, which coincided with slowing of sinus rhythm. Considerable variability in repolarization with very prolonged QT intervals was also observed, as well as intermittent sensing of atrial activity (Figure 1A). Testing of the device showed adequate ventricular pacing thresholds and free-floating lead sensitivity set to the minimum value (0.15 mV); notwithstanding, there was loss of atrial sensing. During monitoring, the patient developed TdP episodes (Figure 1B) through short-long-short sequences that were favored by the intermittent atrial undersensing, sudden sinus bradycardia, and pacemaker hysteresis (nonprogrammable in this model). Following an analysis of the relationship of events, the pacemaker was programmed in VVI at a rate of 70 bpm. The TdP episodes disappeared and the QT interval dropped from 600 ms to 500 ms between the first and third day of pacing (Figure 1C). No other therapeutic measures were taken. Structural heart disease, ionic alterations, and use of QT-prolonging agents were ruled out. Ultimately, an atrial catheter was implanted and a DDD generator replaced. A retrospective analysis of the ECG that led to implantation of the VDD pacemaker showed extremely prolonged QT intervals for the heart rate, with absolute QT values of 620 ms and corrected QT interval (QTc, Bazett formula) of 525 ms (Figure 1D).
Figure 1. A: loss of atrial sensing and mode change from VDD to VVI plus hysteresis (VVI+H) in the first beat after failure, with subsequent alternation of VVI and VDD rhythm. Notice the repolarization variability, with absolute QT intervals between 560 ms and 640 ms. B: monitoring plot showing sudden changes in repolarization mode and variability; note the appearance of a nodular complex with a broad T wave where postdepolarization originates. The short-long-short sequence phenomenon that initiates torsades de pointes is repeated. C: QT decrease from day 1 to day 3 only with VVI pacing at 70 bpm. D: complete atrioventricular block with absolute QT of 620 ms.
Patient 2
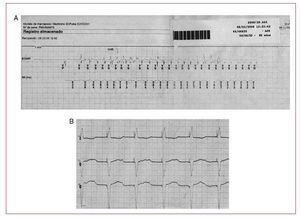
A 78-year-old woman, who had received a VDD pacemaker with tachyarrhythmia capture (Medtronic EnPulse) 15 days earlier for CAVB, presented loss of consciousness with no pulse and was resuscitated by cardiopulmonary resuscitation. The device stored a tachyarrhythmia with variable cycle lengths and morphologies consistent with polymorphic tachycardia (Figure 2A). Pacemaker interrogation showed frequent runs of presyncopal polymorphic tachycardia related to loss of atrial sensing (despite sensitivity set to minimum) and pacemaker switch to VVI mode at the lower pacing limit. Emergency VVI programming at a high pacing rate was required. In addition, at a pacing rate of 60 bpm in this mode, QT intervals of 600 ms were of particular interest (Figure 2B). A 2-chamber implantable cardioverter defibrillator (ICD) with a lower rate limit, programmed at 50 bpm, was ultimately implanted. Over the course of the next 3 years, intrinsic atrial and ventricular rhythm predominated, and no new ventricular arrhythmias were observed. A retrospective analysis of the ECG with CAVB that led to the first implantation showed a measured QT interval of 640 ms and QTc of 575.
Figure 2. A: pacemaker capture consistent with torsades de pointes. B: VVI pacing at 60 bpm with absolute QT of 600 ms.
Patient 3
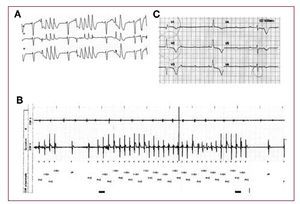
A 72-year-old woman with no structural heart disease received a VDD pacemaker (Guidant Insignia I AVT) for CAVB with proper device functioning at discharge and P-wave sensing of 1.2 V. At 10 days, she consulted for an episode of syncope and several episodes of presyncope and was found to have continual loss of atrial sensing, VVI pacing at 60 bpm, paced QT of 650 ms, and QRS with septal pacing of 135 ms. During monitoring, she presented episodes of nonsustained polymorphic ventricular tachycardia (Figure 3A). Testing of the device showed correct threshold and pacing impedance, with a drop in atrial detection (P wave of 0.4 mV, nominal programmed sensitivity of 0.5 mV). The arrhythmia log showed multiple episodes of irregular ventricular arrhythmia (cycle, 340-390 ms) with an axis change in the ECG (Figure 3B). The pacemaker was programmed in VVI at 90 bpm, which stopped the ventricular arrhythmias. The atrial sensitivity was set to 0.15 ms and the lower pacing limit was retained, which achieved adequate sensing of atrial activity. At 20 months of follow-up, the patient remained asymptomatic and free of arrhythma events. A retrospective analysis of the ECG with CAVB that led to VDD pacemaker implantation showed prolonged QT intervals, QT of 640 ms, and QTc (Bazett) of 450 ms (Figure 3C).
Figure 3. A: runs of polymorphic tachycardia over VVI-paced beat due to sensing failure. B: pacemaker electrocardiograms showing variable ventricular tachycardia. C: complete atrioventricular block with absolute QT of 600 ms.
DISCUSSION
Although the QT is physiologically prolonged in bradycardia, TdP rarely appears. Onset of TdP has been described, however, in 5% to 30% of patients with CAVB.2 In this regard, Kurita et al3 observed that patients with CAVB who developed TdP had abnormally prolonged QT intervals at lower heart rates.
It is not entirely clear why noticeably prolonged repolarization occurs in some patients with bradycardia.
Chevalier et al4 studied the hypothesis of latent genetic alterations and analyzed the genetic prevalence of mutations among the subgroup of patients with CAVB and QT ≥600 ms; these authors found mutations in only 17% of cases. Various limitations described in the study may explain the low prevalence observed. One limitation that is impossible to ignore is the time dependence of the QT interval, namely, that the duration of the CAVB itself noticeably prolongs the QT interval.5
Of note, QT intervals measured in ECGs with CAVB from the 3 patients described showed an absolute value of ≥600 ms in the absence of drugs and ionic abnormalities. Furthermore, time-dependent shortening of the QT interval was documented in patient 1 after VVI pacing at 70 bpm, which shows the importance of time in repolarization remodeling. Therefore, according to the repolarization concept described by Roden et al,6 it is likely that these patients carry a mutation of genes that regulate ventricular repolarization, which has remained subclinical because it is compensated by other ionic currents and only manifests as QT prolongation and onset of TdP under certain stressful conditions (such as the bradycardia in our 3 patients), favored by loss of atrial sensing.
Although a direct relationship between short-long-short sequences and TdP onset was not observed in patients 2 and 3, we believe that RR oscillations must have played a key role. Given the probable predisposition to the onset of TdP in these patients with bradycardia, it is noteworthy that polymorphic tachycardia did not occur during the CAVG episode. In this regard, we believe that bradycardia, which was a result of setting the lower rate to the lowest limit, as well as RR interval irregularity, a result of intermittent atrial undersensing and pacing hysteresis, may have combined to reduce the repolarization reserve and, consequently, lead to TdP.
We believe that the lack of previous descriptions of the problem described in this report may be due to the fact that, along with the low incidence of undersensing,7 a number of conditioning factors must come into play to produce TdP (probable genetic substrate, duration of bradycardia, lower pacing limit programmed, female sex, and other unknown factors).
The QT interval limit at which a patient with CAVB should be considered potentially predisposed to the events described is unknown. Nevertheless, according to the literature, an absolute QT ≥600 ms4 or a Tpeak-Tend>85 ms,8 should raise concern about whether the patient has bradycardia-sensitive repolarization, particularly if the QT continues to be abnormally long with VVI pacing at a normal heart rate of 70 bpm. In this case, good atrial sensing should be attempted in the implant if a VDD system is chosen. The presence of T-wave notches similar to long QT syndrome type II could indicate a risk of TdP.8
In conclusion, before considering defibrillator implantation in patients with a VDD pacemaker who present polymorphic arrhythmias and proven atrial undersensing, the effect of arrhythmogenic drugs, ionic abnormalities, and ventricular dysfunction should first be ruled out. The mechanism presented should then be considered, with careful review of the QT interval of the CAVB episode and QT at slow pacing frequencies. Once the mechanism is identified, slow pacing frequencies should be avoided, and pacemaker hysteresis should not be programmed. These measurements will typically minimize loss of atrial sensing. However, if it is not possible to minimize the detection failure, it may be necessary to implant an atrial lead.
Correspondence:
Dr. V. Palanca.
Servicio de Cardiología. Consorcio Hospital General Universitario de Valencia.
Avda. Tres Cruces, s/n. 46014 Valencia. Spain.
E-mail: palanca_vic@gva.es
Received March 5, 2009.
Accepted for publication May 27, 2008.