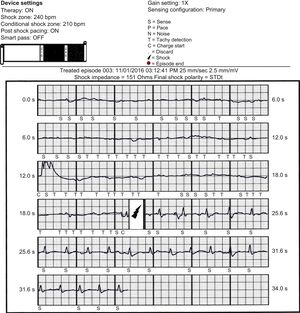
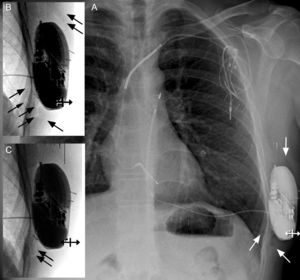
A 41-year-old man with a history of resuscitated cardiac arrest and Brugada syndrome was admitted to our hospital because of lead dysfunction in the internal implantable cardioverter-defibrillator (ICD) implanted 16 years previously. A high shock impedance (> 200Ω) signaled the dysfunction and ICD lead fracture could be observed on X-ray. Due to the risk of ICD lead extraction and the lack of a need for pacing, we decided to abandon the ICD lead and to implant a subcutaneous ICD (S-ICD). During the screening for S-ICD implantation, the sensing was correct in all 3 configurations. The old ICD device was explanted and the lead connectors were sealed with silicone caps. The S-ICD was implanted, creating an intermuscular pocket in the midaxillary line between the anterior surface of the serratus muscle and the posterior surface of the latissimus dorsi muscle.1 The ICD electrode was implanted with the 3-incision technique, with application of a xiphoid and a superior parasternal incision. After the implantation, a defibrillation test was performed, showing a shock impedance of 98Ω. The sensing was suitable in all configurations. Two therapy zones (210 and 240 bpm) were programmed and the primary vector (proximal lead to can) selected for signal detection. The next day, the patient was discharged from the hospital. One hour later, he returned to the hospital because of an ICD shock. He was asymptomatic before and after the episode. S-ICD interrogation showed an electrocardiogram tracing with extremely low voltage, causing inappropriate shock due to ventricular oversensing. After S-ICD shock, sinus rhythm and normal QRS complexes were observed (Figure 1). The shock impedance was increased to 151Ω. The sensing signal was correct in all configurations, at rest as well as during exercise. No dislodgement of the lead or S-ICD was observed on X-ray. However, on close inspection of the postimplant X-ray, a patchy, transparent zone of air was observed covering the S-ICD can (Figure 2A, 2B). The patient was encouraged to walk up and down the ward to promote mobilization of the air. After 2 days, a reduction was observed in the air located at the device pocket (Figure 2C). A defibrillation test was performed, showing a shock impedance of 70Ω. The patient was again discharged home and has remained free of events to date.
Electrocardiogram tracing of the shock episode. A wobbling isoelectric line with ventricular oversensing (S, T) before the discharge and regular QRS complexes (S) after the discharge (arrow) can be seen. The patient was asymptomatic before and after the shock. BPM, beats per minute.
A: antero-posterior chest X-ray after implantation. On close inspection, air entrapment can be seen around the device pouch (white arrows). B: enlargement of device pocket with inverted gray shades (black arrows). C: antero-posterior chest X-ray taken after readmission because of S-ICD discharge. Enlargement of the device pocket with inverted gray shades shows residual air around the S-ICD pocket (black arrows). S-ICD, subcutaneous implantable cardioverter-defibrillator.
Most inappropriate S-ICD shocks occur because of T-wave oversensing or supraventricular tachycardia above the discrimination zone.2 Subcutaneous emphysema or air entrapment in the pacemaker pocket is a known cause of malfunction of unipolar pacemaker systems.3–5 This case illustrates delivery of an inappropriate shock due to air entrapment in the S-ICD pocket. At the end of the implantation, when the patient was in horizontal position, there was correct shock impedance in the measurement taken. However, in the first X-ray, taken when the patient was upright, air entrapment could be seen around the pocket. Mobilization of the patient had likely led to air accumulation between the S-ICD can and the muscle. This decreased the sensing signal (primary vector) and increased the shock impedance. The “Smart Pass” filter of the S-ICD enables the device to use a 9Hz filter up to 40Hz if the signal is above 0.25mV. However, it does not help to reduce baseline wandering, as this is the result of intermittent contact, instability, or the presence of air. Immediately after ICD shock, the sensing was correct. Muscle contraction triggered by the shock may have redistributed the air, improving the contact between the muscle and the ICD can. Zipse et al.6 recently published a case with an electrocardiogram showing a pattern similar to our case, wherein the air entrapment was demonstrated surrounding the distal electrode, leading to 7 inappropriate shocks. They were able to solve the problem elegantly by reprogramming the sensing vector of the S-ICD to the primary sensing vector, thereby excluding the distal electrode. In our case, the reprogramming of the ICD sensing (excluding the ICD can) did not solve the problem due to the high shock impedance. A conservative strategy of mobilizing the patient and waiting 2 days to allow for reabsorption of the air solved the problem. The size, as well as the location, of the S-ICD favors air entrapment in the pocket. This can be avoided by irrigating with saline solution and applying manual compression during pocket closure.
FUNDINGThis work was supported in part by a grant from AGAUR (Agència de Gestió d’Ajuts Universitaris i de Recerca) Ref.: 2014.SGR.471.
CONFLICTS OF INTERESTJ.M. Tolosana and L. Mont are consultants and lecturers for Boston Scientific, Medtronic, St Jude Medical, Biotronik, and Livanova.
We thank Mr. David Montilla from Boston Scientific Inc for technical support.