Percutaneous coronary intervention (PCI) is a well-established treatment for adult coronary artery disease of any cause, although atherosclerotic disease in the main indication. PCI improves both symptoms and survival, especially in patients with acute myocardial infarction. The procedure, however, is much less well established in pediatric patients, in whom it is limited to isolated cases without problems of vessel size.
Atherosclerotic disease is very rare in children and has multiple causes: congenital heart defects, Kawasaki disease, graft vascular disease (GVD) in heart transplant recipients, extrinsic conduit compression causing right ventricular outflow tract obstruction, and occlusion following heart surgery with coronary manipulation such as arterial switch operation (AS) for dextro-transposition of the great arteries (d-TGA) and the Ross procedure in patients with aortic valve disease.1,2
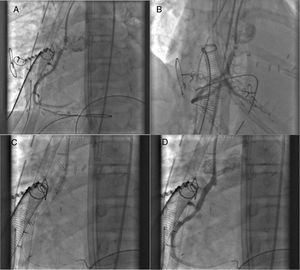
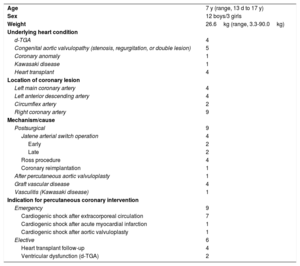
In this letter, we present our experience with PCI performed in patients younger than 18 years at a high-volume center exclusively dedicated to pediatric interventions between 2005 and 2008 (table 1). In this period, 18 procedures were performed in 15 patients with 19 coronary lesions and a mean age of 7 years (range, 13 days to 17 years). Four patients were younger than 1 month and 6 weighed less than 10kg. Ten patients had congenital heart disease: 4 had d-TGA treated with the Jatene ASO and LeCompte maneuver, 5 had congenital aortic valve disease—treated with the Ross procedure in 4 patients (figure 1) and percutaneous aortic valvuloplasty in one—and 1 had a heart anomaly treated with coronary reimplantation surgery. There were also 4 heart transplant recipients with GVD and 1 patient with Kawasaki disease and coronary and cerebral aneurysms.
Characteristics of children and adolescents who underwent percutaneous coronary intervention
| Age | 7 y (range, 13 d to 17 y) |
| Sex | 12 boys/3 girls |
| Weight | 26.6kg (range, 3.3-90.0kg) |
| Underlying heart condition | |
| d-TGA | 4 |
| Congenital aortic valvulopathy (stenosis, regurgitation, or double lesion) | 5 |
| Coronary anomaly | 1 |
| Kawasaki disease | 1 |
| Heart transplant | 4 |
| Location of coronary lesion | |
| Left main coronary artery | 4 |
| Left anterior descending artery | 4 |
| Circumflex artery | 2 |
| Right coronary artery | 9 |
| Mechanism/cause | |
| Postsurgical | 9 |
| Jatene arterial switch operation | 4 |
| Early | 2 |
| Late | 2 |
| Ross procedure | 4 |
| Coronary reimplantation | 1 |
| After percutaneous aortic valvuloplasty | 1 |
| Graft vascular disease | 4 |
| Vasculitis (Kawasaki disease) | 1 |
| Indication for percutaneous coronary intervention | |
| Emergency | 9 |
| Cardiogenic shock after extracorporeal circulation | 7 |
| Cardiogenic shock after acute myocardial infarction | 1 |
| Cardiogenic shock after aortic valvuloplasty | 1 |
| Elective | 6 |
| Heart transplant follow-up | 4 |
| Ventricular dysfunction (d-TGA) | 2 |
d-TGA, dextro-transposition of the great arteries.
A and B, Left anterior and anterior-posterior oblique right coronary angiography views during the immediate postoperative period for a patient treated with the Ross procedure who developed cardiogenic shock and needed extracorporeal membrane oxygenation support. Note the severe stenosis in the ostium of the right coronary artery. C, Drug-eluting stent in the ostium of the right coronary artery. D, Final outcome.
PCI was performed as an emergency procedure in 9 patients with cardiogenic shock, 7 of whom required intervention in the immediate postoperative period after heart surgery. The other 2 procedures were performed after percutaneous aortic valvuloplasty in 1 patient and after acute myocardial infarction in the other (the patient with Kawasaki disease). Extracorporeal membrane oxygen (ECMO) support was required in 8 of the 9 procedures. The other 6 patients underwent elective PCI; 4 were heart transplant recipients with GVD and 2, both with d-TGA repaired with the ASO, had progressive left ventricular dysfunction.
All the procedures were performed under general anesthesia. Femoral access was used in 16 of the 18 interventions; axillary access was required in 2 patients due to iliac-femoral occlusion.
Seventeen of the 19 lesions, mostly located in the ostial-proximal segments, were treated. The 2 untreated lesions were considered to be high-complexity lesions. The procedures were performed using 5-Fr or 6-Fr guiding catheters, usually supported by 0.014“guide wires. Predilation with a semi-compliant or cutting balloon was used in 88.9% of cases and was particularly common in lesions at anastomotic sites. Fifteen stents (9 drug-eluting, 4 bare-metal, and 2 bioabsorbable) were deployed and postdilation with a noncompliant balloon was used in 4 cases. Two lesions were treated with simple angioplasty due to small vessel size (<2mm). Procedural success, defined as a residual lesion of less than 30% and an absence of complications, was achieved in 100% of cases.
There were no procedure-related deaths or major complications. Ventricular function improved in all patients with previous dysfunction. Six of the 9 procedures performed in patients with cardiogenic shock resulted in clinical stabilization (66.7%); the patients were successfully withdrawn from ECMO and subsequently discharged without complications. The 30-day mortality rate was 20% and all the patients who died had refractory cardiogenic shock. The 15 patients were followed up for a mean of 4.7 years. Three patients, all transplant recipients with GVD, underwent repeat coronary angiography, which showed no signs of significant restenosis. Revascularization of a vessel other than the vessel treated at the index PCI was needed in 2 patients due to disease progression.
Although our experience is based on a small, heterogeneous population (with similar characteristics to other series),3–5 we believe that PCI is both feasible and safe for pediatric patients and is a useful option for long-term transplant recipients with GVD and for the treatment of early and late complications of surgical procedures involving coronary manipulation. In such cases, it is important to act as quickly as possible as delays are associated with rapid hemodynamic deterioration, cardiogenic shock, and high mortality risk. All pediatric interventional hospitals must thus be familiar with PCI techniques.