Since the outbreak of the acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the coronavirus disease 2019 (COVID-19) pandemic has spread worldwide and has caused almost 4 million deaths while more than 171 million people have contracted the virus 1 year later.1 It has been previously reported that obesity increases the risk of COVID-19 complications.2 Obesity not only indicates increased subcutaneous adipose tissue, but is also associated with increased visceral ectopic fat, including epicardial adipose tissue (EAT). It is known that increased visceral fat distribution promotes chronic proinflammatory, prothrombotic, and vasoconstrictive states2 and it has been linked to a worse prognosis in COVID-19 patients.3 Due to its local and systemic effects, EAT has been proposed as a leading actor in myocardial inflammation in COVID-19.4,5
Chest computed tomography (CT) examination allows quantification of adipose tissue and assessment of its metabolic activity by measuring its radiodensity or attenuation with a quantitative scale: Hounsfield units (HU). It has been proven that CT attenuation measured in HU can distinguish the metabolic activity of adipose tissue; highly active adipose tissue is characterized by more positive HUs, and hence greater tissue densities.6
Our aim was to investigate the association of EAT attenuation with the clinical outcomes of COVID-19 infection. We retrospectively analyzed EAT attenuation in chest CT scans performed in 75 patients admitted to our hospital due to COVID-19 infection between March and May 2020. The decision to perform the CT scans was made clinically by the treating physician. We compared EAT attenuation values of COVID-19 patients with those of controls individually matched for age and sex. All controls were identified from a prospectively collected database of 3792 patients who underwent a cardiac CT scan in our hospital. The eligibility criteria for controls included 256 patients undergoing the test due to chest pain that were reported as normal (Agatston score=0, normal epicardial coronary arteries and no other pathology seen on the CT scan). After randomly matching for age and sex, we obtained 46 pairs to compare. The study was performed in accordance with the institutional review board of our center, and there was no requirement for informed consent due to the retrospective and observational study design. CT images were analyzed using a state-of-the-art workstation tool (AW Server, General Electric Healthcare, USA). EAT was considered as all tissue with a HU threshold between−190 to−30 contained within the parietal pericardium. EAT attenuation was measured as the mean of 3 values obtained by manually drawing 3 regions of interest: 1 anterior to the great vessels, 1 in the pericoronary fat, and 1 anterior to the right ventricle.
Baseline characteristics of the study cohort were mean age 71±11 years, 56% male patients, and median in-hospital stay of 15 days. Comorbidities were frequent: 55% of patients had hypertension, 27% had a history of cancer, and 25% had diabetes mellitus. A total of 42.7% of patients was overweight and 18.7% obese. Ten patients required intensive care, all of them with mechanical ventilation and 18 patients died (24%).
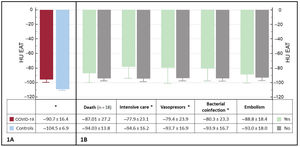
COVID-19 patients had significantly higher EAT attenuation than controls (−91 HU vs−105 HU, P <.001, figure 1A). In our population of cases, we found no differences in EAT attenuation in patients with different cardiovascular risk factors or comorbidities. Regarding the laboratory results, we found no correlation between EAT and any markers (including inflammatory, troponin and D-dimers). EAT attenuation was higher among patients with bacterial coinfection and in those requiring intensive care, mechanical ventilation, and vasopressor support. We found no differences between survivors and nonsurvivors (figure 1B).
EAT attenuation values among different subgroups. A: differences in EAT attenuation between COVID-19 patients and controls. B: relationship between EAT attenuation and prognosis. COVID-19, coronavirus disease 2019; EAT, epicardial adipose tissue; HU EAT, Hounsfield Units in the epicardial adipose tissue. *=P <.005.
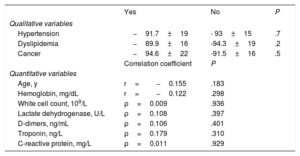
The main factors associated with higher mortality included age, hypertension, dyslipidaemia, prior cancer, baseline hemoglobin, total white cell count, D-dimers, troponin, C-reactive protein, and lactate dehydrogenase levels. Table 1 summarizes their relationship with EAT attenuation values.
Relationship between epicardial adipose tissue attenuation and variables associated with mortality
| Yes | No | P | |
|---|---|---|---|
| Qualitative variables | |||
| Hypertension | −91.7±19 | - 93±15 | .7 |
| Dyslipidemia | −89.9±16 | -94.3±19 | .2 |
| Cancer | −94.6±22 | -91.5±16 | .5 |
| Correlation coefficient | P | ||
| Quantitative variables | |||
| Age, y | r=−0.155 | .183 | |
| Hemoglobin, mg/dL | r=−0.122 | .298 | |
| White cell count, 109/L | ρ=0.009 | .936 | |
| Lactate dehydrogenase, U/L | ρ=0.108 | .397 | |
| D-dimers, ng/mL | ρ=0.106 | .401 | |
| Troponin, ng/L | ρ=0.179 | .310 | |
| C-reactive protein, mg/L | ρ=0.011 | .929 | |
ρ, Spearman's rank correlation coefficient; r, Pearson correlation coefficient.
Our COVID-19 patients had higher EAT attenuation values than controls. Among COVID-19 patients, EAT attenuation was higher in cases with a complicated clinical course: in hemodynamically unstable patients and among those requiring intensive care and mechanical ventilation. These findings are compatible with the hypothesis that EAT could act as a contributor to SARS-CoV-2 entry into the heart and promote an augmented inflammatory response causing myocardial complications, suggested by Kim et al.4 Due to the small population, size we did not perform a multivariable analysis to explore whether this finding is simply a marker of poor prognosis or whether it plays an independent role in the clinical outcome of COVID-19 infection but we found no association between EAT attenuation and the rest of the variables of poor prognosis identified in the series. In addition to the small sample, our study has other limitations: it is retrospective and single-center, it lacks adjustment for confounding, and there was no unified CT protocol. Therefore, our results are difficult to extrapolate to other populations. However, they bring out an interesting univariate association between EAT attenuation and the clinical course of COVID-19 that deserves more research to be fully understood. They also indicate a feasible and easy-to-measure marker available from chest CT that is rarely used in clinical practice and that shows potential to provide prognostic information.
FUNDINGThis work was partially supported by the Regional Health Management of Castilla and León (Gerencia Regional de Salud de Castilla y León): grants GRS COVID 111/A/20, GRS COVID 113/A/20 and GRS COVID 114/A/20.
AUTHORS’ CONTRIBUTIONST. Sevilla, the main and corresponding author, is responsible for the conception and design of the study, analysis of the computed tomography images, refinement of the clinical database, interpretation of the statistical results and drafting of the manuscript. A. Aparisi-Sanz helped with the computed tomography images analysis, the clinical database and reviewed the manuscript. C. Aristizábal-Duque contributed to the computed tomography analysis and reviewed the manuscript. I. Gómez-Salvador performed the statistical analysis and reviewed the draft. C. Baladrón and A. San Román contributed to the study design, interpretation of the results and the final review of the manuscript.
CONFLICTS OF INTERESTThe authors have no relationships relevant to the contents of this paper to disclose.