We present the case of a 54-year-old man referred to our hospital for consideration of endocardial neuromodulation. He had had recurrent presyncope and syncope for more than 10 years and had received a dual-chamber pacemaker 2 years after symptom onset and observation of marked symptomatic sinus bradycardia. Nine years later, on detection of ventricular lead dysfunction and left subclavian artery thrombosis, a new device was implanted via a right access, and the original leads were left in place. The procedure was complicated by cardiac tamponade, so it was decided to remove the device, leaving the patient without pacing support. At the time, given the patient's age and the low ventricular pacing rate, we adopted a watch-and-wait approach. The symptoms, however, persisted (with an average of 2 presyncopal/syncopal episodes a month), and the patient was referred for evaluation of endocardial neuromodulation. After being duly informed, he consented to undergo the procedure and necessary tests and also agreed to the publication of this case report.
The tests performed at our hospital included 24-hour Holter monitoring, which showed no evidence of marked bradyarrhythmia; an exercise stress test, which showed adequate chronotropic competence; and right carotid sinus massage (CSM), which triggered syncope lasting 7.6 seconds (figure 1A). He was diagnosed with cardioinhibitory carotid sinus syndrome and underwent an atropine response test (2mg), which showed an increase of more than 25% in baseline heart rate.
A: syncope with a sinus pause of 7.6s after right carotid sinus massage. B: vagal response to extracardiac stimulation before ablation. C: absence of pauses after carotid sinus massage following ablation of ganglionated plexi. D: absence of vagal response to extracardiac stimulation after ablation. Bpm, beats per minute.
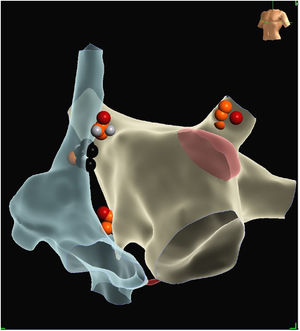
Under sedation with propofol and remifentanil, the patient underwent electroanatomical mapping of the right atrium and superior vena cava using a multipolar HD Grid catheter (EnSite NavX, Abbott, USA). The ablation catheter was then advanced to the right jugular vein for extracardiac high-frequency stimulation (HFS) (10-s bursts, 20Hz at 30V/1ms), which elicited a vagal response with a 3-minute sinus pause (figure 1B). The CSM was still positive with the patient under sedation and was therefore selected as a target for neutralization during the procedure. On completion of electroanatomical mapping of the left atrium, the ganglionated plexi (GP) were ablated using an anatomic approach, with ablation of a) the right superior GP through a right-sided approach (with application of energy to the posteromedial region of the superior vena cava at its intersection with the right superior pulmonary vein) and a left-sided approach in the contralateral region at the anterior level of the right superior pulmonary vein ostium, b) the coronary sinus ostium, c) the left superior GP (at the roof of the left superior pulmonary vein and atrial appendage), and d) the right inferior GP at the level of the right inferior pulmonary vein ostium. On completion of the ablation lesion set, both CSM and HFS continued to show bradycardia, although it was milder than at the beginning and there was no longer any evidence of atrioventricular block. These responses were abolished by additional (bilateral) bursts applied to the area of the right superior ganglion. Following observation of an absence of response to the CSM (figure 1C), the patient was administered 2mg of atropine, which did not lead to an increase in heart rate (figure 1D). As HFS also confirmed an absence of bradycardia (figure 2), the procedure was terminated. Subcutaneous cardiac monitoring showed no episodes of bradycardia (pauses >3s) over a follow-up period of 6 months. The patient also showed clear signs of clinical improvement and was discharged with a subcutaneous event recorder.
Endocardial ablation of GP is an attractive alternative to permanent cardiac pacing for the treatment of symptomatic neurally mediated syncope, particularly in patients with cardioinhibitory responses.1 The technique is still under development, and numerous questions remain to be resolved, such as optimal selection of candidates, choice of best approach (purely anatomic or directed by signs of atrial noncompaction), and definition of clear, specific outcome goals. Pachón et al.2 described the outcomes of catheter ablation in 43 patients with neurally mediated syncope but, like Debruyne et al.,3 who presented a series of 20 patients, they did not include patients with carotid sinus hypersensitivity.
The present case suggests that catheter ablation could prevent pacemaker complications in young patients like ours with carotid sinus hypersensitivity. There has been just 1 report of its use in this setting to date,4 but the authors did not report on specific outcome goals. This is an interesting observation, as patients with carotid sinus hypersensitivity may have a different neurohumoral profile, with normal adenosine levels, unlike patients with syncope without prodrome and sudden atrioventricular block, who typically have low circulating adenosine levels.5
The current case also shows the potential value of CSM for monitoring ablation outcomes; it is a useful point-of-care test, unlike HFS, which requires advancing the catheter to the jugular foramen on repeated occasions and causes discomfort if the patient is not sufficiently sedated. It is noteworthy that persistent bradycardia was observed by both CSM and HSF, and that the responses disappeared almost simultaneously in both tests. This correlation has not been previously reported.
In conclusion, we believe that more studies are needed to evaluate both the long-term efficacy of endocardial denervation of GP in patients with carotid syncope and the prognostic value of CSM responses as a target for neutralization during the procedure.
FundingThe publication of this clinical report is part of a research project funded by a grant from the Asociación del Ritmo Cardiaco de la Sociedad Española de Cardiología for postresidency research training in Spanish hospitals.
Authors’ ContributionsC. Minguito Carazo and M. Rodríguez Mañero prepared and drafted the manuscript. All the authors were involved in the case and contributed to the revision and submission of the manuscript.
Conflicts of InterestNone.